From an outbreak of mysterious lung-injury deaths to America’s near loss of measles elimination status, the beginning of the end of the U.S. HIV epidemic to the Ebola outbreak in the Democratic Republic of the Congo (DRC), CDC worked around the clock – and around the globe – to protect Americans from domestic and global health threats in 2019.
Here’s a closer look at some of the biggest health issues that CDC tackled this year.
Responding to outbreaks and threats
Lung Injuries linked to E-Cigarette use, Vaping, (EVALI)
CDC continues investigating the outbreak of lung injury associated with the use of e-cigarette, or vaping, products, together with state and local health departments and federal partners, such as the U.S. Food and Drug Administration (FDA).
As of December 10, CDC reported 52 deaths and 2,409 cases of hospitalized EVALI by all 50 states, Washington D.C, Puerto Rico, and the U.S. Virgin Islands.
In a breakthrough, CDC laboratories detected vitamin E acetate in the lungs of EVALI patients – direct evidence suggesting that this sticky substance is present in many EVALI cases. Investigation into other possible causes continues.
In September, CDC activated its Emergency Operations Center (EOC) to enhance the inter-agency response to the EVALI outbreak. EOC activation allowed the agency to increase its coordinated operational support for the response to meet the outbreak’s evolving challenges. CDC is providing assistance in epidemiology, disease surveillance, pathologic consultation, clinical guidance development, and communication.
Opioids
Drug overdoses continue to be a major problem across America. There were over 70,000 U.S. drug overdose deaths in 2017, the most recent year for which final data are available. Over two-thirds involved opioids, including heroin and synthetic opioids (such as illicitly manufactured fentanyl and fentanyl analogs). There have also been recent increases in overdose deaths involving cocaine (largely due to contamination with opioids) and methamphetamines and other psychostimulants with misuse potential (both with and without opioids).
The prescribing and dispensing of the overdose-reversing drug naloxone is a critical part of the public health response to the opioid overdose epidemic. Naloxone saves lives – but only if it’s readily available when an overdose occurs. Despite a huge increase in overall prescribing of naloxone, far too little is being dispensed, including in many rural areas of the country where the need is greatest. Moreover, too few doctors are prescribing naloxone to high-risk patients as recommended by CDC’s Guideline for Prescribing Opioids for Chronic Painpdf icon.
As the drug overdose crisis evolves and becomes more complex, CDC is providing $301 million in new Overdose Data to Action funds to states and jurisdictions to align surveillance data with more targeted prevention efforts better. The funds, which will support the work of 47 states, Washington, D.C., Puerto Rico, Northern Mariana Islands, and 16 counties and cities, are part of the Department of Health and Human Services’ Five-point strategy to combat the opioid crisis.
Antibiotic (AR) and Antimicrobial Resistance (AMR)
Antibiotic-resistant (AMR) bacteria and fungi cause more than 2.8 million infections and 35,000 deaths in the United States each year, according to a November 13 CDC report. These are sometimes referred to as antimicrobial-resistant germs.
On average, every 11 seconds someone in the United States gets an antibiotic-resistant (AR) infection – and every 15 minutes, someone dies. When Clostridioides difficile, a bacterium that is not typically resistant but can cause severe diarrhea resulting in death and is associated with antibiotic use, is added to these, the U.S. toll of all the threats exceeds 3 million infections and 48,000 deaths annually.
There were nearly twice as many annual deaths from AR infections as CDC originally reported in 2013. The update comes from previously unavailable data sources. Since then, prevention efforts have reduced deaths from AR infections by 18% overall and by nearly 30% in hospitals. Without continued vigilance, this progress may be challenged by the increasing burden of some infections.
This year, CDC highlighted the success of the yearlong AMR Challenge, an ambitious global initiative to combat the growing threat of AR. Launched in 2018, CDC obtained nearly 350 commitments from 33 countries, pharmaceutical and health insurance companies, food animal producers and purchasers, and medical professionals and healthcare systems to take specific actions to combat antibiotic resistance.
Foodborne Outbreaks
Throughout 2019, CDC investigated and resolved more than 75 outbreaks related to food or animal contact. Notable Salmonella outbreaks were linked to ground beef, raw turkey, pre-cut melons, and papayas. E. coli outbreaks were linked to flour, ground bison, and romaine lettuce. Additionally, there was the largest ever outbreak of Salmonella infections linked to backyard chickens, and an outbreak of drug-resistant Salmonella infections linked to pig-ear dog treats.
During any multistate foodborne disease outbreak, CDC serves as lead coordinator working in close coordination with public health partners to detect the outbreak, define its size and extent, and to identify the source. Public health officials investigate outbreaks to control them, so more people do not get sick in the outbreak, and to learn how to prevent similar outbreaks from happening in the future.
Pregnancy-Related Deaths
A recent Morbidity and Mortality Weekly Report (MMWR) documented persistent racial and ethnic disparities in pregnancy-related deaths. American Indian, Alaska Native, and black women were two to three times as likely to die from a pregnancy-related cause as were white women.
According to a 2019 CDC Vital Signs report, 3 in 5 pregnancy-related deaths could have been prevented. Overall, heart disease and stroke cause more than 1 in 3 pregnancy-related deaths—other leading causes include infections and severe bleeding. The leading causes of death differ by time period throughout pregnancy and after delivery.
Ensuring quality care for mothers throughout pregnancy and the postpartum period can reduce preventable maternal deaths.
Disease Control and Elimination
HIV
Progress in HIV prevention has stalled. Gaps in HIV testing, treatment, and prevention hinder efforts to stop new infections. According to a 2019 Vital Signs report, about 8 in 10 new HIV infections in the U.S. in 2016 came from people not in HIV care. Data also suggest that fewer than 25% of the more than 1 million Americans who could benefit from a daily HIV-prevention pill are using it.
In February, the U.S. Department of Health and Human Services (HHS) proposed the Ending the HIV Epidemic initiative. The plan aims to reduce new HIV infections by 90% by 2030. CDC will play a key role in the proposed initiative, which will leverage critical scientific advances in HIV prevention, diagnosis, treatment, and outbreak response by coordinating the highly successful programs, resources, and infrastructure of many HHS agencies and offices.
Ending the HIV Epidemic aims to achieve maximum impact by first focusing efforts on 48 counties and 7 states; Washington, D.C.; and San Juan, Puerto Rico – where half of HIV diagnoses occur annually – as well as on seven states with a substantial rural HIV burden.
In 2019, HHS, through CDC, awarded $16.5 million to state and local health departments to begin building the foundation for Ending the HIV Epidemic and setting the United States on a path for success.
Measles
This year, there were more U.S. measles cases than in any of the last 25 years. As of December 5, CDC reported 1,276 cases of measles in 31 states for 2019. This is the largest number of cases reported in the U.S. since 1992 (963 cases).
The U.S. maintained its measles elimination status of nearly 20 years after a nearly year-long outbreak in New York City and New York State ended in the fall. The high number of cases in 2019 was primarily the result of a few large outbreaks – one in Washington State and two large outbreaks in New York that started in late 2018, all of them among close, tight-knit communities. Despite high nationwide coverage with the measles, mumps, and rubella vaccine, there are still communities where low vaccination rates leave people vulnerable to these dangerous diseases.
Immunization and Vaccination
According to a 2019 CDC Vital Signs report, nearly two-thirds of pregnant women in the United States have not received the two vaccines recommended during pregnancy for influenza and whooping cough (pertussis). Low rates of vaccination during pregnancy leave expecting moms and babies unprotected and at high risk for hospitalization and even death.
To date, influenza activity for the 2019-2020 season in the United States remains low. Receiving a seasonal influenza vaccine each year remains the best way to prevent seasonal flu. CDC recommends annual influenza vaccination for everyone 6 months and older with any licensed, influenza vaccine that is appropriate for the recipient’s age and health status. In addition to keeping you from getting sick with flu, the vaccine has other benefits including being life-saving for children, protecting pregnant women and their babies, and reducing the risk of a heart attack in people with heart disease.
A recent study published in CDC’s Morbidity and Mortality Weekly Report revealed that an estimated 92% of cancers caused by the human papilloma virus (HPV) could be prevented by the HPV vaccine. CDC recommends that all preteens get the multi-dose HPV vaccine when they are 11 or 12 years old – before they are ever exposed to the virus. However, according to the 2018 National Immunization Survey Teen, only 51% of all teens received all recommended doses of the HPV vaccine.
Domestic Preparedness and Global Health Security
Ebola
As the outbreak in the Democratic Republic of the Congo (DRC) continues, the number of Ebola cases has reached 3,313 and more than 2,204 deaths. To rapidly identify cases and prevent further spread of Ebola, CDC continues to work with the U.S. embassy in DRC to rapidly respond to “hotspots” where the security situation is permissible. CDC also continues to closely coordinate with partners across the Department of Health and Human Services on continuing efforts to fight this outbreak.
In June, CDC activated its Emergency Operations Center (EOC) to support the coordinated inter-agency response to the outbreak in eastern DRC. As of December 13, 2019, CDC staff have conducted 573 deployments to the DRC, neighboring countries, and WHO headquarters. CDC has permanent staff in the three high-risk countries bordering the outbreak (South Sudan, Rwanda, Uganda), including staff in DRC.
DRC has more than 300 graduates of CDC’s Field Epidemiology and Laboratory Training Program who are playing a central role in this public health response.
2020: Looking Ahead
As 2020 approaches, CDC remains vigilant to combat these and other urgent threats. Health threats can arise at any time – at home or abroad – and CDC’s most important mission is always to protect the health of the American public from the unexpected.
To learn more about the work of CDC visit CDC.gov
U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES
CDC works 24/7 protecting America’s health, safety and security.
Whether diseases start at home or abroad, are curable or preventable, chronic or acute, or from human activity or deliberate attack, CDC responds to America’s most pressing health threats. CDC is headquartered in Atlanta and has experts located throughout the United States and the world.







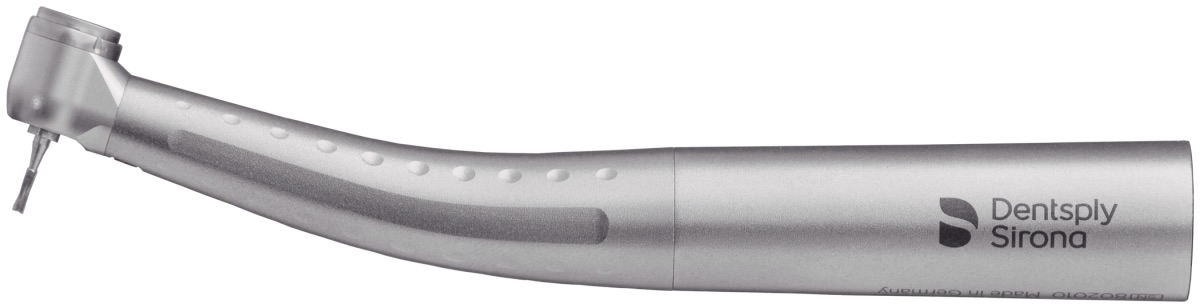
 Dentsply Sirona, the world’s largest manufacturer of professional dental product and technologies, introduces the new Midwest® Stylus Plus Mini highspeed air handpiece. The new design features an improved grip and shorter head to allow deeper access, without compromising performance and durability.
Dentsply Sirona, the world’s largest manufacturer of professional dental product and technologies, introduces the new Midwest® Stylus Plus Mini highspeed air handpiece. The new design features an improved grip and shorter head to allow deeper access, without compromising performance and durability.