Single-Visit Full-Arch Implant-Supported Prostheses
Virtual planning and in-office 3D printing to facilitate immediate provisionalization following implant placement
Rick Ferguson, DMD | Gregori M. Kurtzman, DDS
Virtual planning and 3D printing have revolutionized dental implant treatment. In the past, planning for full-arch treatment was typically done at the laboratory, and stone models with dentures were used to create surgical guides. Later, the incorporation of cone-beam computed tomography (CBCT) permitted virtual planning for implant placement that took the patient's anatomy and its contained structures into consideration. This data was then utilized to conventionally fabricate surgical guides. The next step in the evolutionary process of dental implant treatment was the incorporation of 3D printing, which enabled the in-office fabrication of surgical guides either prior to the surgical appointment or on the same day when time permitted. Then, following implant placement, intraoral scans could be taken to transfer that information to the planning software to design and print provisional hybrid prostheses, allowing patients to leave with accurate, esthetic restorations with minimal time involvement at delivery by dentists and their teams. The following case report outlines the steps for an All-on-X case from virtual planning to guide printing, surgical placement of implants, and fabrication of a provisional hybrid prosthesis.
Case Report
A 59-year-old female patient presented to the practice with failing mandibular and maxillary dental restorations that had been placed outside of the United States. Her mandible had been treated with an implant-retained overdenture (LOCATOR®, Zest Dental Solutions) that had initially been supported by five implants; however, two of the implants had failed prior to her presentation for a consultation and only three remained. The maxillary arch was also a concern, and she expressed a desire to be restored with a fixed approach in both arches. Her maxillary arch was treated first by placement of six implants and the delivery of an immediate 3D printed provisional hybrid prosthesis, and then she returned for the re-treatment of her failing mandibular implant-retained overdenture, which followed the same approach and is the focus of this case report.
Treatment Planning and Guide Fabrication
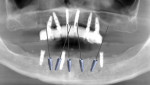
In a CBCT scan that had been acquired to document the patient's upper arch following placement of the maxillary implants and provisional 3D hybrid prosthesis, the panoramic view noted bone loss associated with the remaining mandibular implants (Figure 1). A discussion was had with the patient to review the clinical findings, and the treatment that was recommended involved removal of the remaining three mandibular implants and placement of five new implants that were properly placed to retain a hybrid prosthesis. Following a period of integration, the provisional hybrid prostheses in both arches would be used to fabricate final milled zirconia hybrid restorations. This would allow the patient to "test drive" the esthetics and permit any changes that she desired to be incorporated into the final prostheses. The patient agreed to the treatment plan.
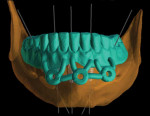
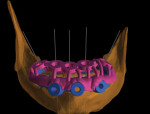
To begin, the CBCT data was imported into implant planning software (Blue Sky Plan®, Blue Sky Bio) for virtual planning. Five implant positions were planned between the mental foramina, with the most bilaterally distal implants tipped distally to spread the emergence and increase the anterior-posterior spread (Figure 2). Each of the planned fixtures would be 3.8 × 10 mm tapered implants (Tapered Pro, BioHorizons).
Next, the patient's existing mandibular overdenture was scanned with an intraoral scanner (Medit i700, Medit) and a replica was designed and printed on a 3D printer (Phrozen Sonic Mini 4K, Phrozen3D) with a custom build plate (Ferguson Mini Stealth Plate, Digital Educators) utilizing a try-in resin (Rodin™ Try-In, Pac-Dent). This was then placed intraorally, and the patient's occlusion and vertical dimension of occlusion were verified. The design file of the replica denture was then imported into CAD/CAM software (DentalCAD, Exocad) and merged with the virtual mandible to permit the design of several guides.
First, a fixation pin guide was designed to predrill for the placement of horizontal fixation pins on the facial aspect of the mandible, which would be utilized to stabilize a bone reduction guide and surgical guide (Figure 3). The fixation pin guide was then printed on the 3D printer using try-in resin (Rodin Try-In, Pac-Dent) and the metal sleeves were inserted (Figure 4). Next, the bone reduction guide was virtually designed using the pin guide holes (Figure 5), and then the surgical guide for the implant osteotomy preparations was virtually designed to engage the stabilized bone reduction guide (Figure 6). After the design was finalized, the bone reduction guide was 3D printed with denture resin (Rodin™ Titan, Pac-Dent) (Figure 7), and the surgical guide was 3D printed with appliance resin (Rodin™ Splint, Pac-Dent) (Figure 8). The metal guide sleeves were then luted to both of these guides using the denture resin. The bone reduction guide and surgical guide were designed to interlock intraorally, providing stability to first reduce the crestal height for a level surface and then guide the creation of the implant osteotomies (Figure 9).
Implant Placement
After the consent form was reviewed and signed by the patient, a local anesthetic was administered by infiltration into the buccal vestibule from distal to the right mental foramen to distal to the left mental foramen. The fixation pin guide was then inserted intraorally, and the patient was instructed to occlude to stabilize it on the arch. Next, a surgical handpiece with a 1.8-mm drill was inserted into each of the three horizontal guide sleaves to create channels for the pins (Figure 10). Following creation of the three fixation pin channels, the guide was removed from the mouth.
Using a scalpel, a crestal incision was made, and a full-thickness flap was elevated with an extension on the facial aspect to below the pin channels that were created. The three failing implants were then explanted, and the sites were debrided of any residual tissue. The bone reduction guide was then inserted intraorally, and the fixation pins were placed to stabilize it intraorally (Figure 11). Once fixated, the bone reduction guide was utilized to guide a bone reduction bur (Surgical Carbide Bur, Meisinger USA) to create a level horizontal crest.
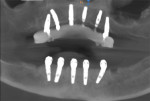
With the bone reduction complete, the surgical guide was inserted intraorally to engage the stabilized bone reduction guide, which would provide stability for the osteotomy preparation (Figure 12). The osteotomies were then created through the guide at the five planned locations utilizing a guided surgery kit (Pro Guided Surgery, BioHorizons) to accommodate the 3.8 mm × 10 mm implants. After the surgical guide was removed from the mouth, leaving the bone reduction guide in place (Figure 13), the implants were placed into the osteotomies (Figure 14).
Multi-unit abutments were then placed onto each of the implants, with 30° angulated ones on the two most distal implants bilaterally and straight ones on the three center implants (Figure 15). Covers were placed onto each multi-unit abutment, and the soft tissue was sutured around them utilizing a polyglycolic acid suture material (Figure 16).
Fabrication and Delivery of the Provisional Prosthesis
Once the soft tissue had been sutured into place, the cover caps were removed, and scan bodies (OPTISPLINT®, Digital Arches) were placed onto each of the multi-unit abutments. The scan bodies were then luted together with a dual-cure composite (OPTIWELD™, Digital Arches), and an intraoral scan was performed (Medit i700, Medit) (Figure 17). To capture the positions of the implants in relation to the opposing arch, the scan bodies were removed, the 3D printed duplicate denture was filled with a monobody impression material (EXAFAST™ NDS Mono-phase, GC America) and inserted intraorally, and the patient was guided into occlusion (Figure 18). The replica denture with the impression was then scanned extraorally and imported into the CAD/CAM software along with the scan of the arch with the scan bodies in place to provide an accurate virtual model for the creation of the provisional hybrid prosthesis (Figure 19).
Using this virtual model, the provisional hybrid prosthesis was designed to eliminate the need for titanium bases by utilizing prosthetic screws with tapered heads (MUA Rosen Screw®, Rosen Implant Solutions) to fixate it to the implants (Figure 20). The provisional hybrid prosthesis was then 3D printed using the denture resin (Figure 21). After the supports were removed, the teeth were stained and glazed with a light-cure staining system (Rodin™ Palette Naturalizing Kit, Pac-Dent), and pink composite (Anaxgum, Anax USA) was applied to the facial aspects of the gingival area and light cured to simulate gingival tissue (Figure 22).
The provisional prosthesis was taken back into the operatory and inserted intraorally. The tapered head prosthetic screws were then inserted into the screw access holes and tightened to 10 Ncm per the manufacturer's recommendations. The occlusion was verified, and the patient was given a mirror to view the esthetics of both full-arch prostheses together (Figure 23 and Figure 24). After a postoperative CBCT scan was acquired to document the positions of the implants, she was dismissed (Figure 25).
The patient will wear the provisional prostheses for a minimum of 5 months to permit the complete osseointegration of the implants and allow her to determine if she would like to make any esthetic changes prior to fabrication of the final restorations. The final restorations, which will be monolithic milled zirconia hybrid prostheses, will follow the design of the provisional prostheses by being retained with tapered head screws to eliminate the need for titanium bases.
Conclusion
Virtual planning and 3D printing facilitate an accelerated treatment workflow within the office when full-arch All-on-X treatment is planned. As the case presented demonstrates, treatment from planning and guide fabrication to implant placement and fabrication of a provisional hybrid prosthesis can be accomplished efficiently and accurately utilizing a digital workflow that includes an in-office 3D printer. This aids in the elimination of fees to outside laboratories as well as delays associated with having guides created and a prosthesis fabricated after implant placement is performed.
About the Authors
Rick Ferguson, DMD
Diplomate
American Board of Oral
Implantology/Implant Dentistry
Director
Implant Educators Academy
Private Practice
Davie, Florida
Gregori M. Kurtzman, DDS
Master
Academy of General Dentistry
Diplomate
International Congress of Oral Implantologists
Private Practice
Silver Spring, Maryland