Trans-Sinus Dental Implants
An alternative to zygomatic implants in the severely edentulous maxilla
Alexandre-Amir Aalam, DDS | Alina Krivitsky-Aalam, DDS
For some implant patients who present with limited bone in the maxillary arch, in order to avoid the need for extensive bone grafting and to provide immediacy in restorative treatment care, zygomatic or pterygoid implants are remotely anchored to the basal bone of the maxilla.1 The clinical utilization of these implants involves a complex process that must be performed by a well-trained and experienced practitioner. They are technique sensitive, can be associated with significant morbidity, and often do not allow for treatment revision if complications arise.2-4
For these reasons, practitioners such as Ole Jensen,5 Paolo Maló,6 Tomas Grandi,7 and those in the authors' group have looked at other surgical procedures that, when indicated and correctly performed, can offer a reliable alternative to zygomatic dental implants in the treatment of the severely edentulous maxilla.8,9
The Trans-Sinus Approach
One of the of the primary advancements in the surgical protocols used as substitutes for zygomatic dental implants is the trans-sinus approach. Trans-sinus implants engage three cortexes: the crestal bone, the sinus wall, and the pyriform aperture, and are indicated in various situations, including the following:
• As an alternative to zygomatic dental implants in cases involving Bedrossian edentulism10,11 in zones 1 and 2, which is associated with an anterior "L" shape of the sinus.12,13
• As a rescue implant when standard tilted implants fail in the premolar region.
• On a classic tilted implant case that does not reach the second premolar/first molar, which compromises the anterior-posterior spread of the implants. Trans-sinus implants will eliminate the distal cantilever and reduce the related mechanical complications.14
• In full cross-arch stabilization cases in which anterior standard implants will be connected with posterior pterygoid implants to reduce the cantilever effect and related mechanical complications.
• When the available bone volume associated with the pyriform aperture for apex anchorage of the implant is 3 mm or more.
• When there is 3 to 5 mm of residual subantral bone, which helps guide the drilling sequence and implant placement without drifting against the anterior wall of the sinus and anchoring into it as well as improves primary and secondary implant stability and crestal bone maintenance in the long term.
Simultaneous Grafting
Authors have discussed grafting the subantral area to support the coronal part of the dental implant when the available bone is less than 4 mm. In the protocol used in the following case,8,9 we recommend simultaneously grafting the sinus in order to provide the patient with redundancy in case of implant failure. This step does not increase morbidity or the treatment time because the creation of a sinus window and careful atraumatic elevation of the Schneiderian membrane are part of the trans-sinus implant placement protocol. The graft material, which is usually placed distally to trans-sinus implants in the molar position, will mature and integrate simultaneously with the traditionally placed dental implants. There are many advantages associated with simultaneous grafting during the placement of trans-sinus dental implants, including the following:
• Supporting the coronal aspect of the ridge and supporting the trans-sinus dental implants (ie, crestal bone maintenance)
• Providing bone in the molar area in case there is a need to place additional implants in the future, which could be indicated due to failure of the trans-sinus implants or the need to improve the anterior-posterior spread of the dental implants or to eliminate distal cantilever
• Providing crestal support when placing zygomatic dental implants, which improves stability and reduces the risk of future oroantral communication related to zygomatic dental implant complications15,16
• Reducing the risk of oroantral communication in cases of trans-sinus dental implant failure
Case Report
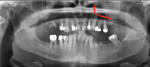
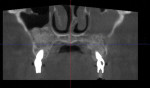
A 65-year-old female patient with an American Society of Anesthesiologists (ASA) physical classification status of ASA II presented with terminal dentition related to the poor periodontal and structural conditions of her remaining teeth. To replace her failing dentition, the patient requested a fixed prostheses for each arch, and she wanted to be temporized in the same manner during the healing phase of the dental implants. A radiographic examination was performed using panoramic radiography and cone-beam computed tomography (CBCT), which revealed that, using the Bedrossian classification, only zone 1 and part of zone 2 had sufficient bone to receive dental implants without extensive sinus augmentation and delayed implant placement (Figure 1). To provide the patient with immediate implant placement and provisionalization and avoid a removable provisional phase, remote anchorage implantology was indicated. In the left quadrant, the anterior wall of the sinus radiographically presented with an L-shaped concave shape, which is well-suited for the use of a trans-sinus implant. The right quadrant had a greater volume of bone, but it was still insufficient for a tilted standard implant; therefore, it was also treatment planned for a trans-sinus implant. The patient agreed to the treatment plan and reviewed and signed the consent forms.
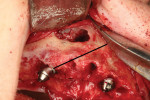
On the day of surgery, a local anesthetic was administered to the maxillary arch from tuberosity to tuberosity as well as to the buccal vestibules and the palatal aspects of the arch. The remaining dentition was extracted, a crestal incision was made, and a full-thickness flap was elevated to expose the buccal ridge to the inferior border of the zygomas, bilaterally. To place the trans-sinus implants, lateral sinus windows were created, the boney windows were carefully removed, and standard sinus lifting techniques were performed, keeping the Schneiderian membrane intact without any perforation. The membrane was dissected from the osseous walls of the sinus and then lifted anteriorly to the mesial border of the canine pillar, medially to the osseous border, and distally to the first molar area. This extended sinus reflection allowed for a safe osteotomy preparation without the risk of tearing the membrane. The implant osteotomy started distal to the second premolar area and then, following the long axis of the canine pillar, went through the crest, traversing the sinus cavity and engaging the cortex of the anterior wall of the sinus, and then finally into the cortex of the nasal floor. Implants that were 25 mm in length were placed bilaterally to achieve such distribution.17 With engagement of the three cortexes, the primary stability of the trans-sinus implants exceeded 50 Ncm. The two axial implants and two pterygoid implants that were placed also demonstrated primary stability that exceeded 50 Ncm, which would permit the delivery of an immediately loaded provisional prosthesis. Multi-unit abutments were connected to the implants. To correct the angulation of the trans-sinus implants, multi-unit abutments with 30° angles were used (Figure 2). Next, platelet-rich fibrin (PRF) membranes, which had been derived from the patient's blood, were placed against the Schneiderian membrane to protect it and to seal any unexpected perforations that could have been missed (Figure 3). The sinus augmentation was then completed with an allograft material (Figure 4), and the window was closed with more PRF membranes (Figure 5), which would prevent soft-tissue invagination as well as promote angiogenesis and blood supply to the grafted bone and thus improve new bone formation into the sinus and adjacent to the dental implant. An effort was made to extend the augmentation area as distal as possible. After tension-free primary closure was achieved (Figure 6), the implant abutments of both arches were scanned for the fabrication of screw-retained full-arch polymethyl methacrylate (PMMA) interim prostheses, and the patient was dismissed.
The provisional prostheses were milled and delivered to the patient within 24 hours (Figure 7 and Figure 8). The occlusion was verified, taking care to obtain a tripodization of occlusal contacts along the prosthesis and eliminate any balancing contacts. In addition, the intaglio surface was checked and corrected to leave space for tissue swelling to occur. A postoperative CBCT scan and panoramic radiograph were acquired to verify proper implant placement, abutment seating, and bone graft placement (Figure 9 and Figure 10).
Conclusion
Trans-sinus dental implants achieve adequate primary stability for immediate loading protocols, provide a good anterior-posterior spread as well as reduce the overall time and cost associated with treating cases involving severely atrophic maxillae. These implants must be cross-arch stabilized to avoid micromotion and excessive unfavorable mechanical loading. In cases that involve a partially edentulous maxilla, a trans-sinus implant must be connected to anterior and distal implants (3 implants minimum) for tripodization and the elimination of micromotion. Although grafting the sinus has been a controversial topic in the literature,5-7,18,19 simultaneous systematic grafting of the sinus performed at the time of trans-sinus implant placement provides redundancy in treatment should the placement of additional implants be required and safety for the anatomical site, reducing the risk of oroantral communication. This technique should be considered as a primary treatment modality for complete maxillary reconstruction in the zone 1 to 2 Bedrossian classification with an anterior L-shaped sinus anatomy. Extensive knowledge of the anatomy and advanced surgical skills (sinus lift, tilted implant concept, etc) are prerequisites to the usage of this technique; therefore, it should only be performed by knowledgeable, skilled, and experienced providers.
About the Authors
Alexandre-Amir Aalam, DDS
Diplomate
American Board of Periodontology
Diplomate
America Board of Oral Implantology/ Implant Dentistry
Adjunct Associate Professor
Herman Ostrow School of Dentistry
University of Southern California
Los Angeles, California
Alina Krivitsky-Aalam, DDS
Diplomate
American Board of Periodontology
Diplomate
American Board of Oral Implantology/Implant Dentistry
Adjunct Associate Professor
Herman Ostrow School of Dentistry
University of Southern California
Los Angeles, California
References
1. Aalam AA, Krivitsky-Aalam A, Kurtzman GM, Mahesh L. The severly atrophic maxilla: decision making with zygomatic and pterygoid dental implants. J Oral Bio Craniofac Res. 2023;13(2):202-206.
2. D'Agostino A, Lombardo G, Favero V, et al. Complications related to zygomatic implants placement: a retrospective evaluation with 5 years follow-up. J Craniomaxillofac Surg. 2021;49(7):620-627.
3. Ramezanzade S, Yates J, Tuminelli FJ, et al. Zygomatic implants placed in atrophic maxilla: an overview of current systematic reviews and meta-analysis. Maxillofac Plast Reconstr Surg. 2021;43:1.
4. Krennmair S, Weinländer M, Forstner T, et al. The influence of different forms of sinus membrane perforation on the prevalence of postoperative complications in lateral window sinus floor elevation: a retrospective study. Clin Implant Dent Relat Res. 2022;24(1):13-23.
5. Jensen OT, Cottam J, Ringeman J, Adams M. Trans-sinus dental implants, bone morphogenetic protein 2, and immediate function for all-on-4 treatment of severe maxillary atrophy. J Oral Maxillofac Surg. 2012;70(1):141-148.
6. Maló P, de Nobre M, Lopes A. Immediate loading of ‘All-on-4' maxillary prostheses using trans-sinus tilted implants without sinus bone grafting: a retrospective study reporting the 3-year outcome. Eur J Oral Implantol. 2013;6(3):273-283.
7. Grandi T, Faustini F, Casotto F, et al. Immediate fixed rehabilitation of severe maxillary atrophies using trans-sinus tilted implants with or without sinus bone grafting: one-year results from a randomised controlled trial. Int J Oral Implantol (Berl). 2019;12(2):141-152.
8. Aalam AA, Krivitsky-Aalam A, Zelig D, et al. Trans-sinus dental implants, for immediate placement when insufficient alveolar height present: an alternative to zygomatic implants - surgical case series. Ann Med Surg (Lond). 2023;85(1):51-56.
9. Holtzclaw D, Aalam AA. Remote Anchorage Solutions for Severe Maxillary Atrophy. Zygoma Partners, LLLP; 2023:409-425.
10. Bedrossian E. Chapter 5: Systematic pretreatment evaluation of the edentulous maxilla. In: Bedrossian E, ed. Implant Treatment Planning for the Edentulous Patient. Mosby; 2010:37-40.
11. Sadowsky SJ, Bedrossian E. Evidenced-based criteria for differential treatment planning of implant restorations for the partially edentulous patient. J Prosthodont. 2013;22(4):319-329.
12. Iwanaga J, Wilson C, Lachkar S, et al. Clinical anatomy of the maxillary sinus: application to sinus floor augmentation. Anat Cell Biol. 2019;52(1):17-24.
13. Agliardi EL, Romeo D, Wenger A, et al. Immediate rehabilitation of the posterior maxilla with extensive sinus pneumatization with one axial and one trans-sinus tilted implant: a 3-year clinical report and a classification. J Prosthet Dent. 2015;113(3):163-168.
14. de Carvalho LP, de Carvalho AM, Francischone CE, et al. Biomechanical behavior of atrophic maxillary restorations using the all-on-four concept and long trans-sinus implants: a finite element analysis. J Dent Res Dent Clin Dent Prospects. 2021;15(2):106-110.
15. Vrielinck L, Moreno-Rabie C, Schepers S, et al. Peri-zygomatic infection associated with zygomatic implants: a retrospective longitudinal cohort study. Clin Oral Implants Res. 2022;33(4):405-412.
16. Sáez-Alcaide LM, Cortés-Bretón-Brinkmann J, Sánchez-Labrador L, et al. Patient-reported outcomes in patients with severe maxillary bone atrophy restored with zygomatic implant-supported complete dental prostheses: a systematic review. Acta Odontol Scand. 2022;80(5):363-373.
17. Zaninovich M. Clinical guidelines for rehabilitation of the severely atrophic maxilla using extended-length subcrestal angulated implants and modified trans-sinus nasal protocol: a case report. Int J Oral Implantol (Berl). 2020;13(3):291-298.
18. Lie SAN, Leung CAW, Claessen RMMA, et al. Implant survival after graftless sinus floor augmentation in highly atrophic maxillae: a randomized controlled trial in a split mouth study. Int J Implant Dent. 2021;7:107.
19. Lie SAN, Claessen RMMA, Leung CAW, et al. Non-grafted versus grafted sinus lift procedures for implantation in the atrophic maxilla: a systematic review and meta-analysis of randomized controlled trials. Int J Oral Maxillofac Surg. 2022;51(1):122-132.