The Immediate Anterior Implant and Provisional Crown
William T. Conklin, BSEE, DDS, DICOI
One of the most challenging procedures in dentistry is the restoration of a single upper central incisor. Complicating this situation are an inadequate crown-to-root ratio, previous endodontic treatment with or without surgical intervention, inadequate periodontal support, presence of the dark triangle, and the adjacent teeth (virgin teeth vs bridge abutment). Occasionally, complete crown fracture causing irreparable damage to the tooth also presents. In the past, treatment to remediate these conditions required removal of the tooth and placement of a fixed or removable prosthesis, which led to an adequate, but not exceptional, outcome. If removal of the tooth is the only option, should dentists let the extraction site heal with or without socket preservation? Should placement of a transitional, nonfunctioning esthetic appliance, either bonded to the adjacent teeth or removable, be an acceptable option during the healing phase?
Recently, a method to solve this problem has been gaining favor. Dentists can now consider placement of an immediate implant, abutment, and transitional crown to stabilize the papillae, as well as the hard- and soft-tissue contours at the time of extraction.
Past treatment options for replacing a missing tooth had some limitations. In the first year of tooth removal, a loss of 25% of the bone width and 4 mm of height could create a compromised edentulous ridge.1 A conventional fixed partial denture would look good for the first year and then could create a gap between the pontic and the tissue. The adjacent teeth also could lose their periodontal support. Over time, patients would have an esthetic failure in the buccal height of contour of the edentulous space. Removable appliances would create a similar situation. Therefore, a long-term outlook must include the preservation of the edentulous ridge.
The following case study addresses this issue and how treatment (at time of extraction) of the residual ridge must be of primary concern. In a study by Schwartz-Arad et al,2 87 patients received a total of 210 provisionalized implants into fresh extraction sites between 2000 to 2005 with a 6- to 52-month follow-up.2 The overall survival rate was 97.6%. Human histologic studies recently completed by Guida et al3 showed that “immediate loading did not seem to impair osseointegration of an immediate post-extraction implant compared to an unloaded post-extraction one.” Guided bone regeneration (GBR) during immediate implant placement also has been found to be an effective treatment modality. Buser et al4 reported that guided bone regeneration into fresh extraction sites with immediate implant placement at 4 to 8 weeks showed successful outcomes for all 45 cases at a 2- to 4-year evaluation. Based on the evidence on immediate implant placement into fresh extraction sites, dentists can use the presented strategy predictably for replacement of a missing anterior tooth.5,6
Case Example
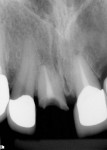
A 46-year-old man presented with a complete horizontal fracture of tooth No. 8, which had been previously treated with a ceramometal crown. The periapical radiograph showed that the tooth had been treated endodontically and had a short anatomical root (unfavorable crown-to-root ratio; Figure 1). The placement of a post and core and new ceramometal crown was contraindicated. The adjacent teeth had recent restorations and no indications for replacement. A computed tomography image (i-CAT®, Imaging Sciences Intl, Hatfield, PA) (Figure 2) of the area revealed a thin buccal plate and emergence of the tooth from the alveolus. The apical palatal shelf presented a sufficient volume of bone to engage an implant. Based on the morphology of the proposed extraction site, it was determined that as well as placement of the implant, GBR would be necessary for maintenance and augmentation of the buccal ridge7 and its potential defect caused by the tooth’s placement in the alveolus. To minimize post-extraction sequelae, a flapless approach to remove the tooth was planned. The use of platelet rich plasma to augment the bone graft material was considered; however, it was not instituted in this case because of the small volume of graft material. The patient was instructed to rinse with chlorhexidine 1 day before the surgery and prescribed 2 g of amoxicillin to be taken 1 hour before the procedure. He was administered 800 mg of ibuprofen at the procedure’s onset. Once successful and profound anesthesia with 2% lidocaine with epinephrine (1:100,000) was achieved, the tooth was removed atraumatically using a straight periotome to separate the periodontal ligament from the boney alveolus and its root surface. With controlled force of the periotome apically and slight widening of the alveolus, removal of the tooth was facilitated without further damage to the existing buccal ridge (Figure 3). Using a periodontal probe, a boney dehiscence of 5 mm from the adjacent facial height of contour of the contralateral tooth No. 9 was detected. (This dehiscence determined the platform height in the socket.)
The roughened surface of the implant should be even or 1 mm apical to the contralateral buccal bone height of contour of the tooth.8 Next, the location of the osteotomy (preparation of the bone for placement of the implant) into the extraction site was determined. Engagement of the apical third of the implant into the alveolus provides the primary stability for immediate loading. To determine the proper engagement, the dentist must consider the palatal vault angle with the alveolar ridge, the width and diameter of the extraction site, emergence of the coronal portion of the tooth incisally from the osteotomy, acceptable length and diameter of the implant, and the platform position located in the post-extraction site.9,10 Prior determination of these variables can be made with a volumetric scan and a preformed splint using radiopaque contrast medium for the replacement tooth. Using an Essix®-type retainer (DENTSPLY Raintree Essix, Sarasota, FL) or vacuum splint, the emergence of the implant can be determined by adjacent teeth (previous tooth position if acceptable or a diagnostic wax-up of the ideal position can be used). For this case, the patient’s crown was used for radiographic measurements. The area of the incisal line angle to the lingual fossa of the central incisor was considered ideal (Figure 4).
The long axis of the osteotomy was placed parallel to the palatal alveolar wall of the extraction site. Initial penetration was started with a No. 6 carbide round bur to engage the apical terminus of the extraction site approximately 1.5 mm palatal to the apex of the tooth. To ensure the proper and subsequent placement of the osteotomy, dissection of the palatal tissue was used to gain access to the alveolar process of the palate. With use of a small elevator, undermining of the buccal tissue was performed concurrently and a visualization of the entire alveolus was facilitated. Using an undersized implant drill (2 mm) and slow speed (50 rpm), apical pressure was placed, with resistance given by the palatal cortical plate in a lateral direction to the predetermined depth. Subsequent and sequential drill sizes were used according to manufacturer’s recommendations to push the osteotomy toward the buccal. It has been reported that 35 Ncm is the safe minimum requirement for immediate loading of the implant.11 To obtain this torque, placement of the apical third of the implant in the existing alveolus and, in this case, the bone density less than 375 Hounsfield units (D4 bone) suggested under drilling the osteotomy site by one diameter size to create a lateral condensation of the trabicular bone on placement of the implant. The implant (12-mm Straumann® Bone Level Implant, Straumann USA LLC, Andover, MA) was initially placed with a power handpiece 1 mm apical to the implant length and then by hand to achieve final alignment and depth. A cover screw was placed onto the implant before the bone graft (Figure 5).
Then, Puros® 0.25 mm to 1 mm cortical allograft material (Zimmer Dental Inc, Carlsbad, CA) was placed into the buccal pouch that was made by undermining the periosteum over the dehiscence and the space created by the extraction site. This graft gave the appearance of a buccal ridge augmentation. It has been noted that up to 2 mm of gap between implant and boney wall will fill in without grafting.12 After the bone condenses into the defects and an oval-shaped contour that takes on a concave shape from the incisal plane develops, the cover screw would be replaced with a screw-retained temporary abutment that was prepared on the implant analog, outside the mouth. The immediate temporary was fabricated to contain the graft material in the extraction site and minimize contact with the oral cavity environment.13 A preformed ion polycarbonate crown (3M ESPE, St. Paul, MN) was trimmed and modified to fit the implant-retained edentulous ridge. To develop the tissue contour of the temporary, a bonding agent was placed inside the temporary crown with a bis-Acryl material (3M ESPE), which was seated over the lubricated abutment (Figure 6). This material would be used to position the temporary crown onto this abutment. With the light-cured material, a convex surface was created to maintain the position of the adjacent papillae, buccal tissue height of contour, and containment of the particulate bone material without the use of a membrane.7
The final temporary must be checked for proper occlusion and elimination from any working, balancing, or centric contact. The patient was sent home with the new tissue-contoured temporary at time of surgery (Figure 7), a prescription for clindamycin 300 mg every 6 hours for 7 days, and postoperative instructions not to chew on the temporary. A 1-week postoperative check-up was scheduled, at which time the site showed remarkable healing (Figure 8).This unloaded temporary would remain out of occlusion for 5 months, allowing for the maturation of the bone graft. It is known that if properly placed, the graft material can augment and reinforce the quality of the natural bone in the socket and around the implant.14 On subsequent follow-up appointments, the temporary was modified to control the tissue contours that developed from the implant–graft–soft tissue complex. With adjustments to the buccal cervical cavosurface of the temporary, the position of the buccal free gingival margin was controlled for matching of the contralateral soft tissue. Bulking out the crown raised the free gingival margin. Under-contouring the crown allowed tissue to fill in the created space (Figure 9). Subsequent appointments revealed a developing and stable periodontium.
Conclusion
The ability to replace a nonrestorable tooth has been a compromise of choice in the past with conventional restorative techniques. The complete replacement of a tooth at the time of extraction with a dental implant and provisional crown now is considered by many to be the treatment of choice. This case study demonstrated the procedure for and implementation of a technique often referred to as the “4 in 1” technique: extraction, implant placement, bone graft, and provisionalization. By completing the implant placement and bone grafting at the time of tooth extraction, the periodontal architecture was maintained, the time required for patient treatment was minimized, and an esthetic emergency on placement of a temporary crown on the immediate implant abutment was circumvented.
References
1. Deporter DA, Watson PA, et al. A clinical trial of a partially porous coated endosseous dental implant in humans: protocol and 6-month results. In: Laney WR, ed. Second International Congress on Tissue Integration in Oral, Orthopedic & Maxillofacial Reconstruction. Chicago, IL: Quintessence Publishing, Inc; 1992.
2. Schwartz-Arad D, Laviv A, Levin L. Survival of immediately provisionalized dental implants placed immediately into fresh extraction sites. J Periodontol. 2007;78(2):219-223.
3. Guida L, Iezzi G, Annunziata M, et al. Immediate placement and loading of dental implants: a human histologic case report. J Periodontol. 2008;79(3):575-581.
4. Buser D, Bornstein MM, Weber HP, et al. Early implant placement with simultaneous guided bone regeneration following single tooth extraction in the esthetic zone: a cross-sectional, retrospective study in 45 subjects with a 2-4 year follow-up. J Periodontol. 2008;79(9):1773-81
5. Misch CE, Wang HL, Misch CM, et al. Rationale for the application of immediate load in implant dentistry: part II. Implant Dent. 2004;13(4):310-321.
6. Misch CE, Suzuki JB. Tooth extraction, socket grafting, and barrier membrane bone regeneration. In: Misch CE, ed. Contemporary Implant Dentistry. 3rd ed. St. Louis, MO: Mosby; 2007:874-878.
7. Petrungaro PS. Replacing the natural tooth system in the esthetic zone: flapless implant placement and simultaneous restoration to preserve tissue contours and guarantee esthetics. Inside Dentistry. 2005;1(2):76-79.
8. Petrungaro PS. Immediate restoration of implants utilizing a flapless approach to preserve interdental tissue contours. Pract Proced Aesthet Dent. 2005;17(2):A-H.
9. Misch CE. Anterior single-tooth replacement: surgical considerations. In: Misch CE, ed. Contemporary Implant Dentistry. 3rd ed. St. Louis, MO: Mosby; 2007:739-766.
10. Testori T, Bianchi F. Ideal implant positioning in a maxillary anterior extraction socket. Academy News. 2003;14(2):1,8.
11. Carr AB, Larsen PE, Papazoglou E, et al. Reverse torque failure of screw-shaped implants in baboons: baseline data for abutment torque application. Int J Oral Maxillofacial Implants. 1995;10(2): 167-174.
12. Froum SJ. Immediate placement of implants into extraction sockets: rationale, outcomes, technique. Alpha Omegan. 2005;98(2): 20-35.
13. The Bio-Col technique. In: Sclar AG. Soft Tissue and Esthetic Considerations in Implant Therapy. Chicago, IL: Quintessence Publishing, Inc; 2003:93-104.
14. Saadoun AP. Immediate implant placement and temporization in extraction and healing sites. Compend Contin Educ Dent. 2002;23(4):309-326.
About the Author
William T. Conklin, BSEE, DDS, DICOI
Private Practice
Windsor, California