Digital Radiography
Dale Miles, DDS, MS
In May 1993, I gave my first invited presentation on digital x-ray imaging at the Computers in Clinical Dentistry Conference in Indianapolis. In October 1993, I published my first article on solid-state detectors.1 Since then I have given more than 120 invited presentations on digital x-ray imaging and integration of systems into the dental office. Early on there were many problems of many different varieties. But now there are no bad digital imaging systems. There are only bad regional levels of support. All of the obstacles (most of which are perceived and not real2) to digital x-ray system adoption have been eliminated. Many dentists I encounter still remain frustrated with a commercial vendor whose local representative has not responded to a problem in the dentist’s office, and bad service is unacceptable. However, despite this single persistent problem, there is now no reason to wait to go digital, or no better time.
Digital radiography has finally matured to the point in which adoption is not an option. It is not a matter of if you are going digital, but when. The number of providers of these systems continues to grow, not decline, and dentists are now routinely moving computers into the operatories. Vendors’ sales staffs have become very knowledgeable, their trainers more skilled and available, and their software tools more robust and useful. There is no better time to buy a digital system than right now. This brief article will outline the latest developments and options in digital radiography.
No shortage of products or innovations
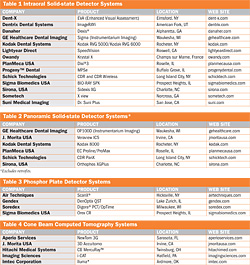
To my best knowledge, at this writing there are 14 solid-state detector systems (Table 1), at least 6 panoramic solid-state systems (Table 2), and 5 persistent phosphor plate receptor systems (Table 3), not including resellers of various digital systems.
The information in Tables 1 through 3 validate the inevitable move to digital technology in our practices. Not only are intraoral and panoramic digital hardware now in most practices, there are even 3-dimensional volumetric imaging devices called cone beam computed tomography (CBCT) machines, which offer incredible images of anatomy, implant sites, and lesions. Figure 1; Figure 2; Figure 3 show images from 3 recent cases from my radiology practice. Table 4 details the CBCT manufacturers. Radiographic interpretation of grayscale images is quickly moving toward radiographic visualization of 3-dimensional color images. What were differential diagnoses have now started to become more precise clinical impressions. Using CBCT or cone beam volumetric imaging (CBVI), disease features and anatomy can be selected and viewed much more precisely than ever before.3-5
In addition to the currently available systems, which range in price from $150,000 to $350,000, the next CBCT system that will come to the dental market will be the upgrade to the existing ProMax digital panoramic machine from PlanMeca Oy (Helsinki, Finland). Although pricing is not yet available, this will be the first (and may be the only) CBCT machine that can be offered to the dentist or dental specialist as an upgrade to his or her existing panoramic machine, which may make CBCT much more available to the general dentist. Currently, most CBCT machines are in radiographic laboratories or specialty private practices. Some machines can also be found in dental schools. Several other manufacturers are developing and this technology for sale to the profession in the near future.
The most recent trend from digital system manufacturers is the customizing of task-specific image processing tools (ie, filters in their software that are useful for a specific application, such as caries detection or bone change in the periapical region). Figure 4 shows an original image and then the same images processed to be inverted and embossed to make disease features more detectable. These 2 filters are common to almost all system software packages whether they are an integrated part of a larger practice management system or a stand-alone image software product.
Figure 5 ( A; B; CView Figure)is a comparison that demonstrates proper use a tool for a specific task. In this case, a film image of caries that is just apparent in the outer enamel on tooth No. 14 has been scanned. The dentinoenamel junction appears intact. Figure 5A is the original scanned image. Figure 5B has had dust and scratches removed in Adobe® Photoshop® (Adobe, San Jose, CA) and optimized for contrast and density. This optimized image has then had an embossing filter applied (again in Photoshop), but with lighting selected to highlight the carious defect. When viewed closely, it can be seen that the lesion does indeed go right to the dentinoenamel junction, and a very early carious lesion on the mesial surface of tooth No. 19 can also be discerned, which is not visible on the original image (white circle). Manufacturers are now improving their software to allow this higher level of image processing.
The hardware of the digital systems is now very reliable. The software tools have been adopted, tested, and used by dentists, and feedback has allowed manufacturers to make their utilities more user-friendly. Software that is optimized for dental tasks, that is intuitive, and that allows dentists to perform feature extractions with more certainty is more useful software. More useful software will in turn result in better clinical decision-making, which will improve patient care. Everyone wins in this scenario, and digital imaging manufacturers and users are now ready to take the technology to the next level—visualization not interpretation of x-ray features.
OTHER INNOVATIONS
Image Optimization by Personal Preference
One rather unique software product offering will come from Dentrix Dental Systems (American Fork, UT) in their next upgrade to Image 4.2. This upgrade will go a long way to making dentists feel more comfortable with digital x-ray image processing. Many dentists are disappointed with the initial image characteristics they see first digitally acquired images. Some do not like the high edge effect (Figure 6), while others cannot decide whether or not the contrast and/or density are optimal for their personal vision. In the 4.2 upgrade, Dentrix has created a start-up task in which the dentist chooses between a pair of images, rejecting either the left or right of the pair until the image viewed is ideal for his or her personal preference. An analogy might be the traditional eye examination during which the patient selects the best option for clarity between 2 lenses until his or her vision is clear through the selected pair of lenses. Thus, Dentrix will customize the initial image displayed to the dentist, based on his or her own decisions, so that the displayed image is close to ideal.
The Super Bitewing
PlanMeca USA (Roselle, IL) has recently introduced 2 new applications for use with their Dimaxis software and digital panoramic x-ray machine (Promax). When acquiring a panoramic radiograph, the operator can select the system’s Interproximality program. Because PlanMeca has a C-arm (a device commonly used in mammography), the machine’s rotation can be started from different points. The significance of this specialized program feature is that it opens the contact points of the premolars so that interproximal carious lesions are now visible on a panoramic image. No other machine can offer this feature. The overlap of interproximal contact points has always been seen as an impediment to using panoramic radiography for cavity detection. This programmable feature eliminates this problem (Figure 7).
In addition to this feature, PlanMeca USA introduced another caries-specific application by creating the Super Bitewing program. Selecting this option allows the dentist to view an enlarged (magnified) pair of bitewing images derived from the Interproximality image capture (Figure 8). Clinicians can judge for themselves whether or not the image quality is sufficient for caries detection.
Conclusion
X-ray imaging will continue to change rapidly. The hardware—solid-state and phosphor receptors, x-ray generators, and computers—are all now very stable and efficient. Training has vastly improved and understanding software tools and their application is gaining momentum. New modalities such as CBCT will continue this digital imaging evolution, and make feature extraction and decision-making more precise and easier to perform. Radiographic interpretation will be replaced by disease visualization.
The numbers of radiographic laboratories will increase as demand for these specialized services grows. The Internet will allow real-time consultation and image and report management to be performed quickly, securely, and efficiently. Implant services, including rapid surgical stent construction and laboratory communication, will also move beyond paper to the Internet.
Advanced digital imaging will drive even more of the procedures performed in dental offices, including rapid model production for prosthodontic and orthodontic needs. One only has to look at what has happened in the past 5 years with 3-dimensional imaging capability to realize that digital imaging is here to stay and total adoption of these tools, both the devices and the software, is inevitable. Plan for it, embrace it, learn about it, and adopt it—digital imaging is not just in your future, it is your future.
References
1. Miles DA. Imaging using solid state detectors. Dent Clin North Am. 1993;37(4):531-540.2. Miles DA, Razzano MR. The future of digital imaging in dentistry. Dent Clin North Am. 2000;44(2):427-438.
3. Miles DA. Digital X-ray imaging for dentistry—the “solid-state” of the art. Available at: https://learndigital.net/solid_state.htm. Accessed April 4, 2006.
4. Danforth RA, Dus I, Mah J. 3-D volume imaging for dentistry: a new dimension. J Calif Dent Assoc. 2003;31(11):817-823.
5. Danforth RA, Peck J, Hall P. Cone beam volume tomography: an imaging option for diagnosis of complex mandibular third molar anatomical relationships. J Calif Dent Assoc. 2003;31(11): 847-852.
 |  | |
| Figure 1 CBCT image of a condylar head and loose body (circle) in joint space. This image was created quickly by using software and reconstructed 3-dimensional data (Accurex Software, CyberMed, Seoul, Korea). | Figure 2 CBCT image of an odontogenic cyst or tumor. Note the resorption (arrow) of the permanent second molar apices by the lesion. The diagnosis was not available at time of writing (Accurex Software, CyberMed). | |
 |  | |
| Figure 3 CBCT image s created for 3-dimensional orthodontic assessment and treatment planning (Accurex Software, CyberMed). | Figure 4 A comparison of software tools. Column A = original image; Column B = inverted image of original; Column C = embossed image filter. | |
 |  | |
| Figure 5A An original image scanned on flat bed scanner. | Figure 5B The same image optimized for contrast/ density and with scratches removed. | |
 |  | |
| Figure 5C The lesion reaching the dentinoenamel junction shown on embossed image. The lesion was not detected in Figure 5A, but made detectable/visible by embossing tools in Photoshop® (Adobe, San Jose, CA). | Figure 6 Although some dentists might think that this image is too digital, it appears to reveal the anatomy very clearly even with its high contrast and high edge effect. (Image courtesy of PlanMeca USA, Roselle, IL.) | |
 |  | |
| Figure 7 This image shows improved contact point visualization in the premolar region. There is some minor overlap between teeth Nos. 4 and 5 and 11 and 12, but otherwise all other contact points are open. (Image courtesy of PlanMeca USA.) | ||
 | ||
| Figure 8 Image areas selected from panoramic radiograph acquired in the Interproximality program, which appear as magnified bitewing radiographs or Super Bitewings. (Image courtesy of Ari Kontkannen, PlanMeca USA.) | ||
| About the Author | ||
 Dale Miles, DDS, MS Dale Miles, DDS, MS Chief Executive Officer Interactive Diagnostic Systems, Inc. Fountain Hills, Arizona Private Practice Fountain Hills, Arizona | ||




