Reconstruction of Sockets and Associated Maxillary Ridge Defect Using Suture Tenting, Synthetic Bone Graft, and Unique Macro Morphology Implants With an Immediately Loaded Provisional Bridge
Dominic O’Hooley, BDS
Abstract: Immediate implant placement in the anterior maxilla remains complex, particularly when the labial cortical plate of the socket is deficient and there is an associated class IV ridge defect with both hard- and soft-tissue deficiencies. This case report describes a novel combination of polydioxanone (PDS) suture tenting to support a synthetic bone graft with simultaneous implant placement with implants featuring a body-shift design and subcrestal internal angle correction. In addition, the implants were immediately loaded with a four-unit provisional bridge at the time of surgery, thus reducing morbidity, costs, and total treatment time.
To achieve predictable, optimized outcomes for immediate implant placement and loading, both prosthodontic and surgical factors must be considered. Among these factors are implant design and 3D position, hard- and soft-tissue quality, primary stability, emergence profile, and esthetics of both the provisional and final restorations.1
After tooth extraction, bony ridge remodeling occurs.2 Immediate implant placement in the esthetic zone, albeit a frequently carried out procedure, does not prevent ridge remodeling after the loss of the periodontal ligament.1,3,4 A variety of techniques have been described to ameliorate this phenomenon.5-12 Techniques have been described to reconstruct type III sockets but do not include immediate tooth replacement therapy.13,14
This article presents a technique to stabilize synthetic particulate bone substitute using resorbable suture tenting, while performing immediate tooth replacement therapy for two teeth, one of which had a class II socket, and immediately loading a provisional four-unit bridge in the maxillary esthetic zone.
Case Report
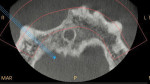
A healthy 64-year-old male patient presented with a failed four-unit maxillary conventional bridge with gross caries affecting both the maxillary right canine and maxillary left central incisor bridge abutment teeth (Figure 1).Upon cone-beam computed tomography (CBCT) analysis, no labial bony wall was detectable for the right canine. The maxillary right lateral and right central incisor pontic sites exhibited both horizontal and vertical bony ridge remodeling (Figure 2 and Figure 3).
After administration of local anaesthesia, both teeth (Nos. 6 and 9) were extracted with the use of both periotomes and forceps. A full-thickness mucoperiosteal flap was raised with vertical releasing incisions mesial to the maxillary right first premolar and maxillary left canine teeth. The surgical site was degranulated using both sharp curettage and degranulation burs. Osteotomies were created and 3.5/4.5 mm x 13 mm implants (Inverta® Deep Conical Co-Axis®, Southern Implants, southernimplants.com) were placed at the right canine and left central incisor socket sites to 60 Ncm insertion torque. Micro-osteotomies were placed at the maxillary right lateral and central incisor pontic sites both on the labial bony plate and the bony crest at the right lateral incisor using a single-use dentin pin drill (Stabilok 0.76 mm, Fairfax Medical Products Ltd.), and polydioxanone (PDS) 2.0 suture (Ethicon PDS II Suture, Johnson & Johnson MedTech, jnjmedtech.com) was used to create tenting for bone graft support both horizontally and vertically (Figure 4 and Figure 5).
Alloplastic particulate bone substitute (EthOss®, Ethoss Regeneration Ltd., ethoss.dental) was placed into the maxillary left central incisor circumferential jumping gap, the maxillary right canine labial dehiscence and jumping gap, the pontic site's horizontally tented ridge deficiency, and the vertically tented ridge deficiency at the maxillary right lateral incisor site. A total of 3 g was used (Figure 6 and Figure 7).
Polyetheretherketone (PEEK) provisional cylinders were placed on both implants to 15 Ncm (Figure 8). A polymethyl methacrylate (PMMA) lab-manufactured provisional four-unit bridge was placed over these and bonded using flowable composite resin. This provisional bridge was finished and polished chairside (Figure 9).
Healing abutments were placed on both implants and the surgical flap was closed transmucosally using polytetrafluoroethylene (PTFE) 4.0 sutures in a tension-free manner. The provisional bridge was screwed onto the implants at 15 Ncm. Careful occlusal analysis followed to ensure the bridge was not in occlusal contact in either centric occlusion or excursions. The patient was given detailed postoperative instructions regarding oral hygiene and an appropriate soft diet.
At 2 weeks, the sutures were removed (Figure 10).
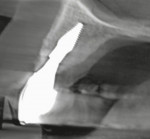
At 7 months, clinical evaluation showed integrated implants with healthy soft issues. Impressions using a custom open tray, splinted impression copings, and addition-cured silicone impression material were taken, and a definitive milled zirconia bridge with milled anodized titanium implant-level abutments was fitted to the implants at 35 Ncm (Figure 11). Post-fitting radiographs were taken (Figure 12).
At 13 months post-surgery, a small-field CBCT was taken and viewed. It showed significant labial bone covering both implants and an improved bony ridge contour at the maxillary right lateral and central incisor pontic sites. Clinical evaluation showed no bleeding on probing with healthy-appearing soft tissues (Figure 13 through Figure 16).
Discussion
Appropriate case selection is essential to achieve optimum results when immediately placing and loading implants in the anterior maxilla.15 The technique presented is indicated in class I and class II sockets and/or class IV ridge deficiencies, where both soft- and hard-tissue augmentations are required.
Careful degranulation of both the sockets and exposed bony ridge was followed by osteotomy preparation, implant placement, micro-osteotomy preparation, and placement of the polydioxanone suture tents. This material resorbs via hydrolysis over 180 to 210 days.16,17
The specific implant macro design used in this case provides a combination of high insertion torque appropriate for immediate loading, along with a narrower coronal portion when compared to a tapered implant with similar maximal width. Combined with the internal screw-access 12-degree angle correction, this enables the implant to be placed less palatal than an implant with a straight connection while still allowing prosthetic screw channel positioning on the palatal of the crown or bridge. Additionally, a circumferential jumping gap is facilitated by the combination of the relatively narrow coronal portion of the implant and its positioning labio-palatally within the bony ridge.6-8
The alloplast particulate bone graft material consists of 65% ß-tricalcium phosphate and 35% calcium sulphate. The calcium sulphate component sets and creates a cell-occlusive barrier, meaning that a separate collagen membrane is not required. The material predictably resorbs over 12 to 18 months to be replaced by host bone.18,19
The present technique is capable of achieving functional and esthetic results predictably using a site-specific implant design, resorbable tenting sutures, and resorbable synthetic bone graft material in synergy.
Conclusion
A technique was presented for the reconstruction of class II and class I sockets in conjunction with a class IV ridge defect and immediate placement and loading of an implant-based four-unit provisional bridge. The case report also showed a tenting technique using resorbable polydioxanone sutures in micro-osteotomies to support a synthetic particulate bone substitute. This presentation is aimed at minimizing surgical interventions, thus reducing morbidity, costs, and treatment time.
About the Author
Dominic O'Hooley, BDS
Fellow, College of General Dentistry (UK); Membership, Faculty of Dental Surgery, Royal College of Surgeons of England; Membership, Faculty of Dental Surgery, Royal College of Physicians and Surgeons of Glasgow; Membership, Advanced General Dental Surgery, Royal College of Surgeons of Edinburgh; Private Practice in Dental Implants, Adel, Leeds, United Kingdom
References
1. Del Fabbro M, Ceresoli V, Taschieri S, et al. Immediate loading of postextraction implants in the esthetic area: systematic review of the literature. Clin Implant Dent Relat Res. 2015;17(1):52-70.
2. Araújo MG, Lindhe J. Dimensional ridge alterations following tooth extraction. An experimental study in the dog. J Clin Periodontol. 2005;32(2):212-218.
3. Botticelli D, Berglundh T, Lindhe J. Hard-tissue alterations following immediate implant placement in extraction sites. J Clin Periodontol. 2004;31(10):820-828.
4. Cosyn J, Eghbali A, Hermans A, et al. A 5-year prospective study on single immediate implants in the aesthetic zone. J Clin Periodontol. 2016;43(8):702-709.
5. Nevins M, Chu SJ, Jang W, Kim DM. Evaluation of an innovative hybrid macrogeometry dental implant in immediate extraction sockets: a histomorphometric pilot study in foxhound dogs. Int J Periodontics Restorative Dent. 2019;39(1):29-37.
6. Östman PO, Chu SJ, Drago C, et al. Clinical outcomes of maxillary anterior postextraction socket implants with immediate provisional restorations using a novel macro-hybrid implant design: an 18- to 24-month single-cohort prospective study. Int J Periodontics Restorative Dent. 2020;40(3):355-363.
7. Chu SJ. Inverted body-shift concept in macroimplant design to enhance biologic and esthetic outcomes: a clinical report. J Prosthet Dent. 2021;126(6):720-726.
8. Chu SJ, Östman PO, Nicolopoulos C, et al. Prospective multicenter clinical cohort study of a novel macro hybrid implant in maxillary anterior postextraction sockets: 1-year results. Int J Periodontics Restorative Dent. 2018;38(suppl):s17-s27.
9. Tsuda H, Rungcharassaeng K, Kan JYK, et al. Peri-implant tissue response following connective tissue and bone grafting in conjunction with immediate single-tooth replacement in the esthetic zone: a case series. Int J Oral Maxillofac Implants. 2011;26(2):427-436.
10. Sanz M, Lindhe J, Alcaraz J, et al. The effect of placing a bone replacement graft in the gap at immediately placed implants: a randomized clinical trial. Clin Oral Implants Res. 2017;28(8):902-910.
11. Chu SJ, Saito H, Östman PO, et al. Immediate tooth replacement therapy in postextraction sockets: a comparative prospective study on the effect of variable platform-switched subcrestal angle correction implants. Int J Periodontics Restorative Dent. 2020;40(4):509-517.
12. Khoury F, Doliveux R. The bone core technique for the augmentation of limited bony defects: five-year prospective study with a new minimally invasive technique. Int J Periodontics Restorative Dent. 2018;38(2):199-207.
13. da Rosa JCM, de Oliveira Rosa ACP, Fadanelli MA, Sotto-Maior BS. Immediate implant placement, reconstruction of compromised sockets, and repair of gingival recession with a triple graft from the maxillary tuberosity: a variation of the immediate dentoalveolar restoration technique. J Prosthet Dent. 2014;112(4):717-722.
14. Zufía J, Blasi G, Gómez-Meda R, Blasi Á. The four-layer graft technique, a hard and soft tissue graft from the tuberosity in one piece. J Esthet Restor Dent. 2019;31(4):304-310.
15. Kan JYK, Roe P, Rungcharassaeng K, et al. Classification of sagittal root position in relation to the anterior maxillary osseous housing for immediate implant placement: a cone beam computed tomography study. Int J Oral Maxillofac Implants. 2011;26(4):873-876.
16. Ooi CP, Cameron RE. The hydrolytic degradation of polydioxanone (PDSII) sutures. Part I: morphological aspects. J Biomed Mater Res. 2002;
63(3):280-290.
17. Ooi CP, Cameron RE. The hydrolytic degradation of polydioxanone (PDSII) sutures. Part II: micromechanisms of deformation. J Biomed Mater Res. 2002;63(3):291-298.
18. Leventis M, Fairbairn P, Mangham C, et al. Bone healing in rabbit calvaria defects using a synthetic bone substitute: a histological and micro-CT comparative study. Materials (Basel). 2018;11(10):2004.
19. Fairbairn P, Leventis M. Protocol for bone augmentation with simultaneous early implant placement: a retrospective multicenter clinical study. Int J Dent. 2015;2015:589135.