Position, Angulation, and Sink Depth: Aspects of Therapy Used to Avoid and Modify Suboptimal Implant Placement
John Cavallaro, DDS; and Gary Greenstein, DDS, MS
ABSTRACT
Careful treatment planning, both clinically and radiographically, and when needed, utilization of a surgical guide, are prerequisites for proper implant placement. Accurate implant insertions with respect to position, angulation, and sink depth facilitate successful fabrication of prosthetic constructs. However, non-optimally located fixtures concerning these three facets of therapy can create biologic and prosthetic complications. This article discusses guidelines for correct implant insertions and for adjustments to surgical and prosthetic protocols to diminish problems associated with suboptimal implant placements.
Precise dental implant placement is a critical component of a successful prosthetic rehabilitation. To achieve good function and esthetics and easy aftercare, careful treatment planning (clinically and radiographically) is required, and a surgical guide should be used as needed. However, suboptimally situated implants in various geometric planes (eg, buccolingually, mesiodistally, apicocoronally) can cause biologic and prosthetic problems.1-3 Accordingly, an implant's position, angulation, and sink depth need to be considered when planning and performing implant surgery. This article addresses criteria for proper dental implant placement and for modifications of routine surgical and prosthetic protocols to compensate for issues associated with less-than-optimal fixture insertions.
Definition of Terms
Implant Position
"Position" refers to the buccolingual and mesiodistal location an implant platform occupies within bone.3 A selected implant site must relate accurately and reasonably to the prosthesis to be constructed. This is accomplished through various methods, such as visual inspection (ie, looking at the central fossae of adjacent teeth in the posterior regions, observing opposing teeth), clinically assessing available bone, and evaluating radiographs or cone-beam computed tomography (CBCT) images. Creation of a surgical guide can be based on mounted casts, wax-ups, a radiographic survey with radiopaque markers, and intraoral scanning techniques (eg, computer-aided design/computer-aided manufacturing [CAD/CAM]).
Implant Positional Zones
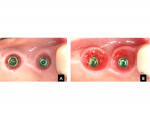
The implant placement zone can be characterized as being located in the central, middle, or peripheral third of the restoration to be fabricated.3 For illustrative and discussion purposes, these areas will be referred to as the green, yellow, and red zones, respectively (Figure 1). Similar to a traffic light, green connotes go ahead with therapy, yellow denotes caution, and red signals danger.
Central zone (green zone): In this zone designation, the border of the implant's platform falls within the central third of the tooth to be restored (Figure 2). This is the optimal position buccolingually and mesiodistally for implant insertion with respect to available bone and the future location of a prosthetic construct.
Middle zone (yellow zone): Here, the periphery of the implant's platform is located in the "para-central" third of the tooth to be restored (Figure 3). This results in a slight malposition buccolingually or mesiodistally (or both) of the implant platform with regard to its ideal location. However, the implant is still located within the confines of the tooth to be restored.
Peripheral zone (red zone): In this scenario, the implant's platform occupies a position at the edge of or outside the tooth to be fabricated (Figure 4). The implant is malposed but may be manageable, depending on its location and the patient's adaptability.
Angulation
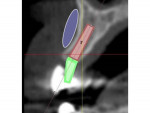
"Angulation" refers to the trajectory an implant follows (relative to a specific reference plane) as it proceeds into the bone (Figure 5).3 Proper implant angulations vary with regard to different intraoral sites. Ideally, maxillary posterior implants are aimed at the opposing tooth's lingual aspect of the buccal cusp.4 For mandibular posterior teeth, the implant is directed at the opposing tooth's buccal aspect of the palatal cusp.4 In the anterior maxilla, an osteotomy's angulation should allow an inserted guide pin to rest in a position similar to a crown preparation for an anticipated cement-retained restoration or approach the lingual aspect of the incisal edge of the opposing tooth for an anticipated screw-retained crown. Maxillary anterior teeth emerge at about a 12-degree angle (an angle formed by the clinical crown axis and a line, which bears 90 degrees to the occlusal plane).5 In the mandibular anterior area, an implant is aimed at the cingulum of opposing maxillary anterior teeth.4 In the mandible, anterior teeth slant labially, premolars are almost vertical, and molars are inclined lingually (15 to 25 degrees).5
Sink Depth
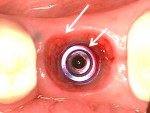
The term "sink depth" denotes the distance between the gingival margin and an implant platform (Figure 6).3 The platform may or may not coincide with the osseous crest, as it can be supracrestal or subcrestal. For bone-level implants placed crestally or subcrestally, biologic width formation (1 mm to 2 mm of epithelial and connective tissue adherence and concomitant bone loss due to its formation) begins at the level of the implant platform.6,7 If platform switching is utilized (eg, an implant-abutment interface that is smaller than the implant platform), the biologic width starts to develop on the implant platform, not at the crest of the ridge, and there is reduced bone loss (approximately 0.5 mm).8 Thus, sink depth affects both the level where biologic width begins to form and the crevicular depth around an implant. The deeper the sink depth, the greater the probing depth adjacent to an implant will be, and this can affect personal hygiene and professional maintenance around the implant.
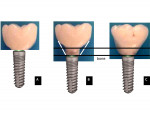
Running Room
Thisis a prosthetic expression that means the same as sink depth. It is measured from the implant platform to the peri-implant soft-tissue margin.3 Running room facilitates a smooth transition from a smaller-diameter, circular-shaped implant platform to the cross-sectional cervical shape of the tooth being restored. This transition is referred to as emergence profile. Increased running room also provides space for tissue sculpting to restore gingival contours. Tissue sculpting is a prosthetic procedure. Acrylic is added to the provisional crown(s) or pontic(s) to induce controlled pressure on the adjacent gingiva, thereby altering its position and/or shape (Figure 7).9,10
Prosthetic and Surgical Adjustments to Accommodate Implants in Different Positional Zones
Central Zone (Green Zone)
Implant placement in the central, or green, zone is the ideal fixture position and should result in a reduced incidence of prosthetic and biologic complications. A benefit of central zone seating usually includes formation of a shallow gingival crevice around the implant (~2 mm to 3 mm), which eases maintenance. Implant insertions in the central zone may permit the use of stock abutments (straight or angled), which is cost efficient. When these abutments do not provide the needed outcome (eg, if there is too much interocclusal space that cannot be managed with a prefabricated abutment, or when an angulated abutment greater than 25 degrees is required, or if a collar height is needed that is greater than provided by the manufacturer), then a custom cast or CAD/CAM abutment can be employed.11
There is another situation when surgical/prosthetic corrections may need to be made in the central zone. An increase in sink depth (1 mm to 2 mm) may be warranted due to a disparity between implant diameter and the prosthetic cross-section of a future restoration. For instance, if an implant has a 4-mm diameter and the tooth to be replaced is 12 mm mesiodistally, then greater sink depth will be needed to provide additional running room to allow for a gradual emergence profile of the crown and provide a hygienic contour (Figure 8 and Figure 9). When a large abutment is necessary, the gingival tissue may need to be incised to facilitate its placement (Figure 10).
It is desirable to place an implant platform 3 mm below the gingival margin.12,13 Especially in the esthetic zone, if the tissue is thin, greater sink depth may be required to hide crown margins. Sometimes in the central zone it is necessary to sculpt the gingival tissue to provide proper gingival form.
In general, implants placed in the green zone have simpler restorative protocols than those located in the yellow or red regions with respect to prosthesis fabrication and try-in and because there is less cement removal, reduced difficulty with screw-access holes, and decreased tissue sculpting. The following dimensions are desirable in the central zone: sink depth 3 mm, running room approximately 3 mm, intracrevicular margin approximately 1 mm, and abutment collar 2 mm tall. In the central zone, abutment-level or implant-level impressions can be used.
Middle Zone (Yellow Zone)
Implant placement in the middle, or yellow, zone may occur due to clinician error or a deficiency of bone causing minor implant malpositioning. This can happen as a result of a practitioner's attempt to avoid bone augmentation procedures. When implants are inserted in the middle zone, dimensions of the final crown remain the same as they would in the green zone despite the fixture not being directly in the middle of the restoration (Figure 11). However, a consequence of middle zone positioning is the potential need for more hardware (abutment, restoration, or a combination of both). This often occurs on the buccal aspect to compensate for a slight lingual implant seating. After an extraction, additional hardware often is needed on the buccal, because the ridge tends to resorb more on the facial aspect of the alveolar ridge compared to the lingual side due to its thinness.14,15 Implant malpositioning in the yellow zone can be modified with an angled or custom abutment, and increased sink depth is used to provide a better emergence profile. This situation usually necessitates an implant-level impression.
Implant insertions in the yellow zone may also require soft-tissue sculpting to achieve appropriate gingival topography. A technique to pre-empt yellow zone placement due to a bone deficiency is to perform guided bone regeneration before or during implant insertion, thereby allowing the implant to be situated in the central zone. Adequate preplanning and the use of a surgical guide can help avoid implant insertions in the yellow zone.
Peripheral Zone (Red Zone)
Red zone implant placements are challenging to manage and can be reviewed from two perspectives: (1) situations in which a fixture either is about to be misplaced or has already osseointegrated, and repositioning (or removal if osseointegrated) is advised, and (2) making adjustments to assuage difficult issues associated with red zone insertions.
In the peripheral, or red, zone a malposed implant in the mesiodistal plane that encroaches on an adjacent tooth or implant ought to be repositioned at the time of insertion. To decrease bone loss and interdental papillae problems, the distance between an implant and a tooth should be 2 mm,16 while the distance between implants should be 3 mm.17 Platform switching may reduce bone resorption between a tooth and an implant if they are too close to each other,18 but the space for a papilla remains compromised. In addition, an implant too close to a tooth or another implant may impede impression-taking because of a lack of enough space for impression copings (impression components can be modified in these situations). In the red zone, an inserted implant that encroaches on the buccal or lingual bony plates also needs to be repositioned, because it may induce bone resorption and recession.1,19 This is particularly true in the esthetic zone with respect to the buccal aspect of the ridge.3
If a red zone seating is projected to occur due to a deficiency of bone, a bone augmentation procedure is recommended prior to or in conjunction with implant insertion. After bone augmentation, the implant's periphery should be at least 1 mm away from the bony ridge's border to diminish the chance of bone resorption.19-22
Some accommodations can be made for red zone implant positioning. Leaving an implant in the red zone has consequences: the restoration will be larger than normal because it is out of position, it will require a custom abutment, tissue sculpting may be necessary, and a test period with a provisional crown may be needed before the final restoration is placed (Figure 12). The rehabilitation may necessitate that alterations of adjacent tooth dimensions (crowns) be made to be compatible with the oversized malposed implant restoration. Slightly reducing the size of a crown may be possible by using only metal lingually or interproximally without porcelain or another surfacing material.
If the restoration requires additional bulk on the lingual or palatal aspect, tongue interference must be assessed. This can be evaluated when the patient wears a provisional prosthesis. The patient needs to be informed in advance that conformative dentistry is being performed and the prosthesis's positioning is not ideal. If an inserted fixture is unacceptable to either the patient or the clinician, removing or submerging the fixture may be necessary. In addition, implants may need enhanced hygienic efforts due to the restoration's size and position. In some situations, an extremely malposed implant (eg, mesiodistally) can be used. For instance, for a malposed implant that is situated in the prosthesis's interproximal area, a crown can be screw-retained (Figure 13). However, this may result in increased thickness of the prosthesis at that location. In general, it may be easier for a patient to adjust to red zone implants when reconstructive dentistry is being performed for a segment or an entire arch, because all the prosthetic contours are under the clinician's control. In this regard, a bulky new prosthesis may be a superior option for a patient who has limited choices and strongly desires a fixed implant solution rather than a removable overdenture, a complete denture, or extensive (ie, multiple) grafting procedures.
Positional errors can be avoided by using digital software for treatment planning and to generate a surgical guide to help execute precise implant placement. In addition, before initiating therapy, bone and soft-tissue issues should be noted and their remedies preplanned.
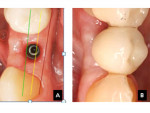
Rectifications and Justifications for Misangulated Implants
Angulation errors in the mesiodistal and buccolingual directions generally are easier to correct than positional errors. When assessing the trajectory of an implant, the clinician should notice the position of adjacent teeth, implants, and relevant anatomy. Although an implant may be placed in its correct position, its buccolingual or mesiodistal angulation may be skewed. This can cause a minor (0 to 15 degrees) or a larger (>25 degrees) misangulation. An implant angulation of 15 degrees can be easily fixed with an angled component. Larger misangulation rectifications may be correctable with either an angled component or a custom-made (CAD/CAM) abutment. Angulating an implant to stay within a bony ridge is common practice. For instance, when there is a sloping maxillary ridge in the bicuspid area, it is advantageous to keep the implant within the alveolar bone to avoid the need for an additional bone augmentation procedure (Figure 14). Abutment angulations of 15 degrees and 25 degrees can laterally adjust the occlusal position of a crown 1.5 mm and 2.5 mm, respectively.3 However, this does not change the implant's gingival position. To compensate for an intentional or unintentional misangulation, the implant's sink depth should be increased 1 mm to 2 mm greater than normal to provide additional running room to develop a gradual emergence profile. Otherwise, this can result in a circumferential ridge lap, which may make hygiene difficult. Angulated abutments also are used to parallel abutments on angled implants that support splinted crowns or a fixed prosthesis.3 However, there are limits to correcting implant misangulations, and clinicians need to avoid alveolar bone fenestrations, ridge dehiscences, and excessive angulations that may not be restorable.
From a mechanical perspective, increased abutment angulations result in a greater amount of stress on prostheses and the surrounding bone than straight abutments.23,24 However, studies do not demonstrate a significant decrease in prostheses' longevity or increased bone loss or additional screw loosening associated with angled abutments.25-28 Also, implants with increased angulations do not demonstrate increased bone loss when compared to straight implants.29
Sink Depth Concerns: Modifications of Surgical and Prosthetic Procedures
In general, implants should be placed as shallow as possible and as deep as necessary. However, numerous issues should be considered when planning the apicocoronal location of an implant, including interocclusal clearance, bone level, tissue thickness, implant malposition or misangulation, impact of adjacent extractions, and the appropriate amount of prosthetic running room.
Interocclusal Clearance and Bone Levels
Prior to implant insertion, the vertical space required to accommodate an implant's restoration needs to be measured.30 For example, a porcelain-fused-to-metal cementable single restoration requires around 7 mm of clearance between the implant platform and the opposing dentition (1.5 mm to 2 mm for porcelain, 4.5 mm abutment height, 0.5 mm crown metal).31 Reduced interocclusal distance of 4.5 mm to 5 mm dictates the need for a screw-retained restoration.30,32 If there is less than 4.5 mm occlusal clearance between the osseous crest and the opposing dentition, a ridge reduction can be performed (if there is adequate bone height),33,34 or the opposing dentition can be selectively equilibrated to provide adequate restorative space. Another choice is to increase sink depth to ensure there is enough interocclusal clearance for a crown. From a different perspective, if there is advanced bone and soft-tissue loss and the patient is not a candidate for augmentation procedures, increased interocclusal clearance can be managed with pink restorative materials at the cervical region of the crown(s) (Figure 15).35
Gingival Thickness
Increased sink depth results in increased probing depths. Therefore, when the restoration is not in the esthetic zone and there is excessive gingival height, consideration should be given to reducing the tissue height. This decreases probing depths and facilitates hygienic measures. However, it is recommended to maintain at least 2 mm of soft-tissue thickness to avoid additional bone loss associated with thin tissues after implant placement.36
Malpositioned and Misangulated Implants
As previously mentioned, implant misangulations and minor implant malpositions can be improved by using angulated abutments, custom abutments, and increased sink depth (1 mm to 2 mm) to facilitate better emergence profiles (Figure 6 through Figure 9).
Extractions
Extractions using a flap routinely result in 1 mm to 2 mm vertical bone resorption and an even greater reduction of ridge width (>3 mm).37,38 In contrast, flapless extractions manifest less reduction of bony ridge width (1 mm).39 If multiple teeth are removed there is increased osseous resorption compared to a single extraction.37,38,40 Thus, if an implant is placed into an extraction socket (immediate implant), or next to a site undergoing an extraction, or in between two extraction sites, sink depth should be increased 1 mm to 2 mm to accommodate expected bone loss.3
Insufficient Sink Depth
If implants are placed without adequate sink depth, it could result in a lack of running room, unfavorable emergence profile, and facial metal abutment display.3 The restoration may look like a mushroom (Figure 8, b) or require the use of a ridge lap, and both situations can cause hygienic issues. To compensate for this, an abutment-restoration with a short transgingival section (UCLA-type) can be placed, or the abutment can be prepared subgingivally. In this situation, if the tissue is thin, facial gingival discoloration may be evident.
Excessive Sink Depth
Sometimes with immediate implant insertion, sink depth is too great due to an attempt to attain primary stability. This causes increased probing depths and possibly maintenance issues. To avoid this at the time of implant seating, the clinician should determine if a wider fixture could be inserted that achieves primary retention more coronally, thereby reducing sink depth. Note, with increased sink depth, crown margins should not be placed too deeply, because this can influence the amount of undetected residual excess cement after delivery of a cement-retained implant restoration.41 A screw-retained restoration may be the superior choice in this scenario. With increased sink depth there also may be issues associated with seating impression copings or other components.
Conclusion
Attention to implant position, angulation, and sink depth is essential when treatment planning and executing an implant case. These considerations can enhance patient satisfaction and minimize prosthetic aftercare issues. Application of knowledge with respect to prosthetic and surgical changes to accommodate placement errors can convert an unfavorable situation to a favorable one. Ultimately, proper planning prevents poor peri-implant and prosthetic performance.
ACKNOWLEDGMENT
Figures 9, 10, 12, and 13 have been reproduced with permission from Cavallaro J, Greenstein G. Prosthodontic complications related to implant placement. In: Froum SJ. Dental Implant Complications: Etiology, Prevention, and Treatment. 1st ed. Wiley-Blackwell: 2010;156-171.
ABOUT THE AUTHORS
John Cavallaro, DDS
Former Clinical Professor, College of Dental Medicine, Columbia University, New York, New York; Private Practice (ret.), Surgical Implantology and Prosthodontics, Brooklyn, New York
Gary Greenstein, DDS, MS
Former Clinical Professor, College of Dental Medicine, Columbia University, New York, New York; Private Practice, Surgical Implantology and Periodontics, Freehold, New Jersey
REFERENCES
1. Chen ST, Buser D, Sculean A, Belser UC. Complications and treatment errors in implant positioning in the aesthetic zone: diagnosis and possible solutions. Periodontol 2000. 2023;92(1):220-234.
2. Cooper LF. Prosthodontic complications related to non-optimal dental implant placement. In: Froum SJ, ed. Dental Implant Complications: Etiology, Prevention, and Treatment. 2nd ed. Hoboken, NJ: Wiley-Blackwell; 2016:539-557.
3. Cavallaro J, Greenstein G. Prosthodontic complications related to implant placement. In: Froum SJ, ed. Dental Implant Complications: Etiology, Prevention, and Treatment. 1st ed. Hoboken, NJ: Wiley-Blackwell; 2010:156-171.
4. Cavallaro J, Greenstein G. Immediate dental implant placement: technique, part 2. Dent Today. 2014;33(2):94,96-98.
5. Misch CE, Bidez MW. Occlusal considerations for implant supported prosthesis: implant protective occlusion. In: Misch CE, ed. Dental Implant Prosthetics. St. Louis, MO: Elsevier Mosby; 2005:472-507.
6. Hermann JS, Schoolfield JD, Nummikoski PV, et al. Crestal bone changes around titanium implants: a methodologic study comparing linear radiographic with histometric measurements. Int J Oral Maxillofac Implants. 2001;16(4):475-485.
7. Hartman GA, Cochran DL. Initial implant position determines the magnitude of crestal bone remodeling. J Periodontol. 2004;75(4):572-577.
8. Atieh MA, Ibrahim HM, Atieh AH. Platform switching for marginal bone preservation around dental implants: a systematic review and meta-analysis. J Periodontol. 2010;81(10):1350-1366.
9. Zamzok J. Avoiding ridge laps through nonsurgical soft tissue sculpting on implant restorations. J Esthet Dent. 1996;8(5):222-228.
10. Spyropoulou PE, Razzoog M, Sierraalta M. Restoring implants in the esthetic zone after sculpting and capturing the periimplant tissues in rest position: a clinical report. J Prosthet Dent. 2009;102(6):345-347.
11. Karunagaran S, Paprocki GJ, Wicks R, Markose S. A review of implant abutments-abutment classification to aid prosthetic selection. J Tenn Dent Assoc. 2013;93(2):18-23.
12. Saadoun AP, LeGall M, Touati B. Selection and ideal tridimensional implant position for soft tissue aesthetics. Pract Periodontics Aesthet Dent. 1999;11(9):1063-1072.
13. Cooper LF. Objective criteria: guiding and evaluating dental implant esthetics. J Esthet Restor Dent. 2008;20(3):195-205.
14. Ferrus J, Cecchinato D, Pjetursson EB, et al. Factors influencing ridge alterations following immediate implant placement into extraction sockets. Clin Oral Implants Res. 2010;21(1):22-29.
15. Barros RRM, Novaes AB Jr, Papalexiou V. Buccal bone remodeling after immediate implantation with a flap or flapless approach: a pilot study in dogs. Int J Dent Implants and Biomaterials Titanium. 2009;1(1):45-151.
16. Esposito M, Ekestubbe A, Grondahl K. Radiological evaluation of marginal bone loss at tooth surfaces facing single Brånemark implants. Clin Oral Implants Res. 1993;4(3):151-157.
17. Tarnow DP, Cho SC, Wallace SS. The effect of inter-implant distance on the height of inter-implant bone crest. J Periodontol. 2000;71(4):546-549.
18. Vela X, Mendez V, Rodriguez X, et al. Crestal bone changes on platform-switched implants and adjacent teeth when the tooth-implant distance is less than 1.5 mm. Int J Periodontics Restorative Dent. 2012;32(2):149-155.
19. Chen ST, Darby IB, Reynolds EC. A prospective clinical study of non-submerged immediate implants: clinical outcomes and esthetic results. Clin Oral Implants Res. 2007;18(5):552-562.
20. Albeshri S, Greenstein G. Significance of facial bone thickness after dental implantations in healed ridges: a literature review. Compend Contin Educ Dent. 2021;42(9):528-535.
21. Monje A, Roccuzzo A, Buser D, Wang HL. Influence of buccal bone wall thickness on the peri-implant hard and soft tissue dimensional changes: a systematic review. Clin Oral Implants Res. 2023;34(3):157-176.
22. Buser D, Monje A, Urban I. Anatomical and surgical factors influencing the outcome of GBR procedures. In: Buser D, ed. 30 Years of Guided Bone Regeneration. 3rd ed. Batavia, IL: Quintessence Publishing; 2021:93-112.
23. Clelland NL, Gilat A, McGlumphy EA, Brantley WA. A photoelastic and strain gauge analysis of angled abutments for an implant system. Int J Oral Maxillofac Implants. 1993;8(5):541-548.
24. Brosh T, Pilo R, Sudai D. The influence of abutment angulation on strains and stresses along the implant/bone interface: comparison between two experimental techniques. J Prosthet Dent. 1998;79(3):328-334.
25. Eger DE, Gunsolley JC, Feldman S. Comparison of angled and standard abutments and their effect on clinical outcomes: a preliminary report. Int J Oral Maxillofac Implants. 2000;15(6):819-823.
26. Balshi TJ, Eckfeldt A, Stenberg T, Vrielinck L. Three-year evaluation of Brånemark implants connected to angulated abutments. Int J Oral Maxillofac Implants. 1997;12(1):52-58.
27. Sethi A, Kaus T, Sochor P. The use of angulated abutments in implant dentistry: five-year clinical results of an ongoing prospective study. Int J Oral Maxillofac Implants. 2000;15(6):801-810.
28. Sethi A, Kaus T, Sochor P, et al. Evolution of the concept of angulated abutments in implant dentistry: 14-year clinical data. Implant Dent. 2002;11(1):41-51.
29. Agliardi E, Clericò M, Ciancio P, Massironi D. Immediate loading of full-arch fixed prostheses supported by axial and tilted implants for the treatment of edentulous atrophic mandibles. Quintessence Int. 2010;41(4):285-293.
30. Carpentieri J, Greenstein G, Cavallaro J. Hierarchy of restorative space required for different types of dental implant prostheses. J Am Dent Assoc. 2019;150(8):695-706.
31. Dozíc A, Kleverlaan CJ, Meegdes M, et al. The influence of porcelain layer thickness on the final shade of ceramic restorations. J Prosthet Dent. 2003;90(6):563-570.
32. Binon PP. Implants and components: entering the new millennium. Int J Oral Maxillofac Implants. 2000;15(1):76-94.
33. Ahuja S, Cagna DR. Classification and management of restorative space in edentulous implant overdenture patients. J Prosthet Dent. 2011;105(5):332-337.
34. Phillips K, Wong KM. Vertical space requirement for fixed-detachable, implant-supported prosthesis. Compend Contin Educ Dent. 2002;23(8):750-756.
35. Coachman C, Salama M, Garber D, et al. Prosthetic gingival reconstruction in a fixed partial restoration. Part 1: introduction to artificial gingiva as an alternative therapy. Int J Periodontics Restorative Dent. 2009;29(5):471-477.
36. Linkevicius T, Apse P, Grybauskas S, Puisys A. The influence of soft tissue thickness on crestal bone changes around implants: a 1-year prospective controlled clinical trial. Int J Oral Maxillofac Implants. 2009;24(4):712-719.
37. Covani U, Cornelini R, Barone A. Bucco-lingual bone remodeling around implants placed into immediate extraction sockets: a case series. J Periodontol. 2003;74(2):268-273.
38. Lekovic V, Kenney EB, Weinlaender M, et al. A bone regenerative approach to alveolar ridge maintenance following tooth extraction: report of 10 cases. J Periodontol. 1997;68(6):563-570.
39. Job S, Bhat V, Naidu EM. In vivo evaluation of crestal bone heights following implant placement with ‘flapless' and ‘with-flap' techniques in sites of immediately loaded implants. Indian J Dent Res. 2008;19(4):320-325.
40. Caneva M, Salata LA, de Souza SS, et al. Influence of implant positioning in extraction sockets on osseointegration: histomorphometric analyses in dogs. Clin Oral Implants Res. 2010;21(1):43-49.
41. Linkevicius T, Vindasiute E, Puisys A, Peciuliene V. The influence of margin location on the amount of undetected cement excess after delivery of cement-retained implant restorations. Clin Oral Implants Res. 2011;22(12):1379-1384.