Novel “All in 4-4-4” Hybrid Prosthesis: Bridging the Affordability Gap
Lambert J. Stumpel, DDS; E. Armand Bedrossian, DDS, MSD; N. Cory Glenn, DDS; Joe Mehranfar, DMD; and Marta Revilla-León, DDS, MSD, PhD
Abstract: A strong body of scientific evidence indicates that a four dental implant-supported prosthesis is well suited for a full-arch rehabilitation. Yet, countless edentulous patients who could benefit from this established concept are left untreated because of high costs. This article describes a novel workflow that enables the fabrication of a metal-resin fixed hybrid prosthesis supported on four implants, with a variable cost for parts and material of around $400 and a (laboratory) production time of approximately 4 hours. This approach allows for the possibility of delivering a final or long-term provisional restoration on the day of implant placement. Because of the relatively low cost and the feasibility of in-house production, this workflow can potentially allow more patients to access high-quality full-arch implant care.
With millions of people having lost all of their teeth in one or both arches, dental implants have proven to be an effective modality in restoring dental functionality. Yet many fully edentulous people do not receive the care that could prevent them from being, to coin a phrase from the late professor Per-Ingvar Brånemark, "dental cripples." A main reason for this is finances. The economic reality is that for most of these patients, this care is outside of their budget.
The dental profession has made tremendous strides in making dental care more predictable, esthetic, and successful overall. However, despite these advances, dental care has not necessarily become more accessible. A simplified economic model to assess the variable cost breakdown for full-arch implant care could comprise the cost of parts and hardware and the hours spent delivering the care. Controlling costs in this model would be aided by reducing the hard cost of the number of parts used and lowering the acquisition cost of these parts, while the variable cost of skilled labor may be controlled by minimizing the number of hours required to deliver the care and simplifying the level of skill needed to do so. In other words, to increase treatment accessibility, providers need to be able to spend less money on parts and have more efficient systems both clinically and in the dental laboratory.
This article describes what the authors call the "All in 4-4-4" workflow that facilitates the fabrication of a full-arch hybrid prosthesis on four implants, costing approximately US $400 for parts and materials, and requiring 4 hours of labor. It also allows for same-day delivery as implant placement, if desired.
Supporting a Fixed Complete Denture
While new technology is creating opportunities in dentistry that were unimaginable just a few years ago, a thorough understanding of established science is needed first and foremost. The scientific literature overwhelmingly shows that just four splinted implants are needed to support a fixed complete denture, and that additional implants do not offer better outcomes. This concept was introduced more than 20 years ago as the All-on-4® concept.1 The foundation for this concept, though, was laid many years before by the Swedish group of researchers who introduced osseointegration to the world.2 These authors stated that the tendency of some clinicians to install as many implants as possible in fully edentulous patients "should be seriously questioned." Since then, many publications support the four-implant concept,3-6 and to the present authors' knowledge, there are no publications that refute it. Some clinicians are of the opinion that more implants should be used as security (eg, "all-on-4 is none-on-3"). However, such an approach is not supported by the scientific literature. Employing additional implants, plus abutments, cylinders, and screws, all of which must be purchased and installed, does not offer a better outcome and will increase costs.
Placing four implants is a first step and is the first "4" in the All in 4-4-4 treatment.
The objective of treatment of edentulism is to provide "teeth." The prosthetic reconstruction in the early days of full-arch implant treatment was typically a cast gold framework supporting denture teeth that was designed for removable dentures and polymethyl methacrylate (PMMA) resin. This hybrid prosthesis was more accurately described as a metal-resin implant fixed complete denture. To this day manufacturers do not rate their denture teeth for fixed reconstructions, yet the dental profession has used them for this purpose for more than 50 years. Chipping, wear, and staining over time must be expected, and patients should be informed that every 5 to 7 to 10 years the acrylic and denture teeth will need to be replaced. To use an analogy, just as a car will need new tires, there is no need to buy a new car every time the tires wear out.
The cast gold framework has mostly been replaced by a milled computer-aided design/computer-aided manufacturing (CAD/CAM) metal framework. An appropriate supporting framework is still needed to support the restorative material.7-9 Today's dental materials generally are not strong enough to withstand occlusal forces, especially after spending some time in the mouth and undergoing moisture and temperature degradation.10 The strongest, least esthetic zirconia might be an exception. There appears to be growing interest in the more esthetic, but lower-strength, zirconia with a supporting metal structure.11 The fabrication of a customized CAD/CAM metal framework is most often performed in centralized production facilities, as relatively few dentists have the required subtractive or additive metal technologies in house. The framework requires multiple days to produce and ship, and the cost of this customized work is appropriately considerable.
New Developments
Recent developments include the introduction of a modular, prefabricated system (Quikbar, QuikBar®, quikbar.net) that allows for the construction of a customized supportive metal framework for a four-implant fixed prosthesis.12 With this system, one set consistent of nine parts is adequate to design a bar on four implants in any possible configuration and size (Figure 1 through Figure 3). The prefabricated parts are purposely larger than needed so they can be cut to size, then bonded together with a chemically and mechanically adhesive composite resin. Bonding metal to metal is a highly reliable and long-standing construction method in dentistry.13-15 Once formed, the bar is then similarly bonded to titanium cylinders. The finished bar is passive to the model and appropriately supportive for the overlaying restorative material. This overlaying material can be any of a number of currently available materials, such as PMMA, composite resin, or zirconia. A moderately skilled technician should be able to fabricate the supportive metal bar, following the manufacturer's instructions, in 20 to 40 minutes. The cost is approximately $300 for the bar components, cylinders, and screws, and an additional $30 to $40 for the composite bonding resin, for a total of around $340, as per the manufacturer.
As previously mentioned, earlier restorative materials were removable denture teeth and PMMA resin. This combination performed together for many years, albeit with some issues related to wear, as noted earlier. Zirconia was introduced with the aim of improving on the denture teeth concept. The strongest zirconia is not highly esthetic, hence the use of veneering porcelain to improve the esthetics was proposed. Unfortunately, the veneering porcelain proved susceptible to chipping.16 More translucent zirconia products were developed, and this treatment modality has increased in popularity. As mentioned, a metal framework is increasingly used to support the more esthetic but inherently weaker zirconia material.A more recent development is the substrative CAM of PMMA resin material. PMMA produced under ideal industrial conditions will yield maximized material properties. It is even possible to mill a pink/white puck to produce a monolithic denture with white teeth and pink papillae (eg, Ivotion, Ivoclar, ivoclar.com). This material is rated by the manufacturer for removable dentures, so when used in a fixed restoration one must expect future wear. Due to its monolithic construct, the failure mode will likely differ from conventional denture teeth and PMMA.
The rapid development of 3D resin printing in additive manufacturing is of great interest in the dental profession. One of the most recent developments is the introduction of resins designed specifically for the production of permanent crowns. Multiple manufacturers have developed ceramic nanofilled hybrid resins for this purpose. When the filler content is more than 50%, these resins can even be considered ceramic restorations following the April 2023 updated American Dental Association definitions (Current Dental Terminology, https://www.ada.org/en/publications/cdt/glossary-of-dental-clinical-terms#cdt). While it is too early to have long-term data, the material properties appear very promising for the application at hand. If the material is strong enough for one crown, it may be logical to think it is strong enough for 14 crowns. This may be especially so for monolithic crowns interconnected and supported by a metal framework. Because production is fast and relatively inexpensive, it opens an opportunity for in-office production instead of using an external centralized production facility. The printing volume for this type of restoration, including print supports, varies between 10 ml and 30 ml of resin. With the cost of these permanent crown resins at $1.50 to $2.00 per ml, the total cost is estimated to be between $15 and $60 per prosthetic arch. When adding this to the cost for parts and bonding resin cited above (approximately $340), the total material cost is about $400. This represents the second "4" in the All in 4-4-4 concept.
Digital Denture Design
With the exception of conventional denture teeth and PMMA, all other restorative materials for full-arch prostheses can be part of a digital production process. While they are all CAM capable, they are first CAD. CAD/CAM has taken over most dental prosthesis manufacturing, with some pockets of analog support. Although the dental laboratory industry has been at the forefront of CAD/CAM utilization, individual dental offices are increasingly embracing the design component. This is mostly because CAM manufacturing is so easily in-sourced with 3D printing. Numerous design software products are available, and after a learning curve, a moderately skilled designer should be able to design a digital denture over a bar substructure in about 15 to 30 minutes. Because the software doesn't know there is a metal bar underneath, a "taco shell" denture can be designed utilizing the most basic software module. Although one can design and produce the pink and white parts independently, it may be easier to produce the complete denture in white and just add pink resin where needed later.17
To initiate the digital design process, the patient's oral situation first needs to be captured and duplicated outside of the oral cavity. While intraoral scanning is increasingly popular, the prevailing literature shows that dependably registering dental implants in a full-arch case is still challenging.18,19 To overcome this drawback of intraoral cross-arch precision, extraoral photographic registration has been proposed. With an extraoral capturing device, photogrammetry registers scan flags that are positioned on the dental implants. This only captures dental implant position; the soft tissue and bite registration will still need to be captured otherwise. Photogrammetry has not been proven superior to analog techniques, and while it may work in many situations, it unfortunately may not work in some, which is problematic in any workflow.20,21
A simple multifunctional registration device, ie, a free, open-source 3D-printed jig that allows the combined registration of implant position, soft-tissue contour, vertical height, and bite registration, was previously described in detail.22 In summary, a rigid, dimensionally stable base is perforated to allow temporary cylinders attached to the abutments to peek through. These cylinders are connected to the base with a dual polymerizing composite resin (eg, SmarTemp® Dual-Cure, Parkell, parkell.com). This assembly registers the implant positions and can be immediately used as a verification jig by performing the one-screw Sheffield test.23 In this concept, one tightens all screws with maximum finger tightness, then loosens three of the four screws. Subsequently, the operator attempts to additionally tighten the remaining screw. If the screw does not rotate, a passive fit can be assumed. The pitch of an M2 prosthetic screw is 0.4 mm. One full rotation would indicate a 0.4-mm gap; consequently, a quarter turn signifies a 100-µm gap. The vertical height is subsequently set by adding and/or subtracting to the central registration pin (Figure 4). Next, the soft tissue is impressed by injecting polyvinyl siloxane (PVS) material between the base of the jig and the soft tissue (Figure 5). Lastly, a stiff PVS bite registration captures the bite at the previously established correct vertical position. All of this verified registration can be accomplished in 15 to 20 minutes at a minimal cost. This assembly can subsequently be used in the laboratory to fabricate the provisional or final prosthesis.
The impression will need to be transformed into a dental cast; dental stone has long been used for this purpose. Due to its volumetric expansion, time involvement, and general messiness, Stumpel described an alternative method to the use of dental stone (Figure 6 through Figure 8).24 In summary, laboratory analogs are tightened into the registration cylinders. Vaseline is applied onto the VPS impression material of the registration and a 2-mm to 3-mm thick layer of thin VPS material is placed in the intaglio. Upon setting, the analogs are bonded with a dual polymerizing composite resin (SmarTemp Dual-Cure) to a dimensionally stable 3D-preprinted base. This base is open source and freely available (quikbar.net/publications-and-downloads/). Next, a stiff PVS putty material is used to complete the volume. Upon setting, the cast can be easily trimmed with scalpels. This precision model takes 10 to 15 minutes to produce. The bar will be fabricated on this cast, and they will be scanned together for the digital component of the workflow.
The design of the prosthesis is performed within a dedicated dental CAD program (eg, exocad Rijeka 3.1, exocad, exocad.com). The Standard Triangle Language (STL) file of the final design is printed with a vat 3D printer (NextDent 5100, NextDent, nextdent.com) in a dedicated resin (saremco print Crowntec, Saremco, saremco.ch) approved for long-term intraoral use. Pink composite resin is applied to simulate gingival tissues. The "taco shell" denture is bonded onto the bar, and the intaglio surface is hand-finished with the same 3D printing resin. The total time involved to fabricate the cast and bar, scan, and design, print, and finish the prosthesis is about 4 hours. This is the third "4" in the All in 4-4-4 concept.
In selected cases, the ability to produce a definitive or long-term provisional prosthesis on the same day as the implant placement may allow for the omission of a provisional restoration and delivery of an immediate final prosthesis. It has been 25 years since the Brånemark Novum® concept was introduced,25,26 with the idea to deliver a final prosthesis on the day of implant placement, reducing costs to allow more patients the benefits of dental implant therapy. The novel concept described herein follows-up on that original concept. Two clinical cases demonstrating this technique are presented.
Clinical Case 1
A 75-year-old female patient presented with a mandibular two-implant-supported overdenture, which she received approximately 1 year prior. She requested treatment to transfer to a fixed restoration. Two additional implants were placed, and her existing overdenture was used to fabricate a resin fixed provisional prosthesis.
Upon verification of osseointegration after the healing period, the approved provisional was used to fabricate a precision cast as described above. The opposing complete denture was captured with an intraoral scanner (TRIOS 3, 3Shape, 3shape.com), and the bite was also captured. The provisional prosthesis was placed onto the precision cast, and this assembly was scanned. Titanium cylinders were secured onto the multi-unit laboratory analogs (Multi-Unit Tall Titanium Base, Preat, preat.com), and the appropriate components (Quikbar) were selected and adjusted to fit (Figure 9). The titanium surfaces were readied for bonding by air-particle abrasion. A dual polymerizing 10-methacryloyloxydecyl dihydrogen phosphate (MDP)-containing composite resin (PANAVIA™ SA, Kuraray, panaviacements.com) was used to bond the metal parts together (Figure 10). Because a curing light will only reach the exterior surfaces, a chemical component is needed for adequate curing. Once the bar was established, it was similarly luted to the titanium cylinders. The bar was then adjusted and shaped with rotary instruments (Mizzy Heatless Wheels, Keystone Industries, keystoneindustries.com).
A thin layer of the MDP-containing bonding resin was applied to the buccal and occlusal portions of the bar, after which an opaquing composite (Anaxblend Opaquer, Anaxdent, anaxdentusa.com) was applied (Figure 11). The bar/cast assembly was scanned. In both the scan of the cast and provisional and the scan of the cast with the bar, the cast is the stable factor. This allows the software (exocad Rijeka 3.1) to align both scans. Digital cross-mounting is a great advantage in digital workflows. In this case, the work order was set to anatomic pontic with gingival design for teeth Nos. 19 through 30. This instructs the software to deliver a preset workflow. The three interrelated scans-opposing complete denture prosthesis, cast with provisional, and cast with bar-were loaded into the software. The software asked the user to define the surface of the scan with the bar. Next, it asked to develop a block-out model; the setting was 0.25 mm and 0-degree undercut (Figure 12). Next, the tooth setup was completed, and then cutback of the base, interproximally and occlusally, was performed (Figure 13). The next step was the design of the gingiva (Figure 14).
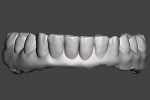
Upon completion of these steps, the final STL file was generated. The finished STL file was loaded into a freely available STL modification program (Autodesk Meshmixer, meshmixer.com) (Figure 15). The surface that was to be colored pink was selected ("S") and reduced by 0.5 mm ("D", normal, 0.5) (Figure 16). The modified STL file was saved, and this file was subsequently 3D-printed in a resin rated for permanent oral use (saremco print Crowntec). Post-processing was done per the manufacturer instructions. The "taco shell" denture was bonded onto the bar with the MDP-containing bonding resin (Figure 17). The intaglio was completed by hand-application of the printing resin. An intensely colored resin (Anaxgum Paint red, Anaxdent) was hand-applied for highlights (Figure 18) and covered with a pink denture base resin (NextDent Denture 3D+, NextDent). The pink resin flowed easily to complete the contours. The resin was hand-polished per the manufacturer's instructions, and the final prosthesis was delivered to the patient (Figure 19 and Figure 20).
Clinical Case 2
A 60-year-old female patient had received four zygomatic implants to support a fixed prosthesis. The workflow to fabricate the permanent metal-resin fixed hybrid prosthesis was similar to the one previously described. Although the resin was monolithic in nature (with multi-color printing being a development expected in the future), the final esthetics were enthusiastically approved by the patient, and the final prosthesis was delivered (Figure 21 through Figure 23).
Conclusion
There is a long-standing, solid body of scientific evidence affirming that a four dental implant-supported prosthesis is well suited for a full-arch rehabilitation. Although this well-established concept has over the years helped many edentulous patients feel "normal" again, millions who could benefit from this treatment have remained untreated because of lack of finances. Reducing overall cost would greatly benefit them. This article introduced the All in 4-4-4 hybrid prosthesis concept: a fixed full-arch reconstruction supported by four dental implants, costing $400 in materials, and needing just 4 hours of laboratory labor to produce.
Disclosure
Dr. Stumpel is the developer of Quikbar. The other authors had no disclosures to report.
About the Authors
Lambert J. Stumpel, DDS
Private Practice, San Francisco, California
E. Armand Bedrossian, DDS, MSD
Affiliate Assistant Professor, Division of Graduate Prosthodontics, Department of Restorative Dentistry, School of Dentistry, University of Washington, Seattle, Washington; Private Practice, San Francisco, California; Fellow, American College of Prosthodontists
N. Cory Glenn, DDS
Director of Clinical Technology, Blue Sky Bio, LLC, Winchester, Tennessee
Joe Mehranfar, DMD
Clinical Director, Implant Education Company; Private Practice, Phoenix, Arizona
Marta Revilla-León, DDS, MSD, PhD
Affiliate Assistant Professor, Division of Graduate Prosthodontics, Department of Restorative Dentistry, School of Dentistry, University of Washington, Seattle, Washington; Faculty and Director of Research and Digital Dentistry, Kois Center, Seattle, Washington; Adjunct Professor, Department of Prosthodontics, School of Dental Medicine, Tufts University, Boston, Massachusetts
References
1. Maló P, Rangert B, Nobre M. "All-on-Four" immediate-function concept with Brånemark System implants for completely edentulous mandibles: a retrospective clinical study. Clin Implant Dent Relat Res. 2003;5(suppl 1):2-9.
2. Brånemark PI, Svensson B, van Steenberghe D. Ten-year survival rates of fixed prostheses on four or six implants ad modum Brånemark in full edentulism. Clin Oral Implants Res. 1995;6(4):227-231.
3. de Luna Gomes JM, Lemos CAA, Santiago Junior JF, et al. Optimal number of implants for complete-arch implant-supported prostheses with a follow-up of at least 5 years: a systematic review and meta-analysis. J Prosthet Dent. 2019;121(5):766-774.e3.
4. Toia M, Stocchero M, Corrà E, et al. Fixed full-arch maxillary prostheses supported by four versus six implants with a titanium CAD/CAM milled framework: 3-year multicentre RCT. Clin Oral Implants Res.2021;32(1):44-59.
5. Maló P, de Araújo Nobre M, Lopes A, et al. The All-on-4 concept for full-arch rehabilitation of the edentulous maxillae: a longitudinal study with 5-13 years of follow-up. Clin Implant Dent Relat Res. 2019;21(4):538-549.
6. Soto-Penaloza D, Zaragozí-Alonso R, Penarrocha-Diago M, Penarrocha-Diago M. The all-on-four treatment concept: systematic review. J Clin Exp Dent. 2017;9(3):e474-e488.
7. Coltro MP, Ozkomur A, Villarinho EA, et al. Risk factor model of mechanical complications in implant-supported fixed complete dentures: a prospective cohort study. Clin Oral Implants Res. 2018;29(9):915-921.
8. Valenti C, Federici MI, Masciotti F, et al. Mechanical properties of 3D-printed prosthetic materials compared with milled and conventional processing: a systematic review and meta-analysis of in vitro studies. J Prosthet Dent. 2022;S0022-3913(22)00415-2.
9. El Samahy MM, Abdelhamid AM, El Shabrawy SM, Hanno KI. Evaluation of physicomechanical properties of milled versus 3D-printed denture base resins: a comparative in vitro study. J Prosthet Dent. 2023;129(5):797.e1-797.e7.
10. Bakir L. Fatigue in dentistry: a review. Biomat J. 2022;1(6):12-21.
11. Stumpel L, Haechler W. The metal-zirconia implant fixed hybrid full-arch prosthesis: an alternative technique for fabrication. Compend Contin Educ Dent. 2018;39(3):176-181.
12. Stumpel LJ. A prefabricated modular substructure for a 4-implant-supported fixed complete denture: a dental technique. J Prosthet Dent. 2020;124(6):637-641.
13. Stumpel L, Quon SJ. Adhesive abutment cylinder luting. J Prosthet Dent. 1993;69(4):398-400.
14. Stumpel L. The adhesive-corrected implant framework. J Calif Dent Assoc. 1994;22(2):47-53.
15. Baldin Able F, de Mattias Sartori IA, Thomé G, Moreira Melo AC. Retrospective, cross-sectional study on immediately loaded implant-supported mandibular fixed complete-arch prostheses fabricated with the passive fit cementation technique. J Prosthet Dent. 2018;119(1):60-66.
16. Papaspyridakos P, Lal K. Computer-assisted design/computer-assisted manufacturing zirconia implant fixed complete prostheses: clinical results and technical complications up to 4 years of function. Clin Oral Implants Res. 2013;24(6):659-665.
17. Stumpel LJ. An analog intermezzo in a digital workflow. Compend Contin Educ Dent. 2020;41(10):536-542.
18. Waldecker M, Rues S, Rammelsberg P, Bömicke W. Accuracy of complete-arch intraoral scans based on confocal microscopy versus optical triangulation: a comparative in vitro study. J Prosthet Dent. 2021;126(3):414-420.
19. Kernen F, Schlager S, Seidel Alvarez V, et al. Accuracy of intraoral scans: an in vivo study of different scanning devices. J Prosthet Dent. 2022;128(6):1303-1309.
20. Zhang YJ, Qian SJ, Lai HC, Shi JY. Accuracy of photogrammetric imaging versus conventional impressions for complete arch implant-supported fixed dental prostheses: a comparative clinical study. J Prosthet Dent. 2023;130(2):212-218.
21. Revilla-León M, Rubenstein J, Methani MM, et al. Trueness and precision of complete-arch photogrammetry implant scanning assessed with a coordinate-measuring machine. J Prosthet Dent. 2023;129(1):160-165.
22. Stumpel LJ. An open-source multifunctional registration device for implant-supported complete dentures. J Prosthet Dent. 2021;125(4):592-596.
23. Jemt T. Failures and complications in 391 consecutively inserted fixed prostheses supported by Brånemark implants in edentulous jaws: a study of treatment from the time of prosthesis placement to the first annual checkup. Int J Oral Maxillofac Implants. 1991;6(3):270-276.
24. Stumpel LJ. In-office fabrication of a definitive cast and duplication of an interim implant-supported fixed acrylic resin complete denture. J Prosthet Dent. 2017;118(2):135-139.
25. Brånemark PI, Engstrand P, Ohrnell LO, et al. Brånemark Novum: a new treatment concept for rehabilitation of the edentulous mandible. Preliminary results from a prospective clinical follow-up study. Clin Implant Dent Relat Res. 1999;1(1):2-16.
26. Engstrand P, Gröndahl K, Ohrnell LO, et al. Prospective follow-up study of 95 patients with edentulous mandibles treated according to the Brånemark Novum concept. Clin Implant Dent Relat Res. 2003;5(1):3-10.