Advances in Esthetic, Immediate Tooth Replacement Therapy Aimed at Improving Clinical Outcomes
SPECIAL REPORT: Implants/Regeneration
Barry P. Levin, DMD
The criteria for successful tooth replacement in the esthetic zone is comprehensive and often complex. Merely achieving osseointegration is no longer the bar that clinicians strive to reach in this endeavor. Achieving and maintaining hard- and soft-tissue stability as well as physiologic, scalloped soft-tissue architecture to frame cosmetic restorations is the ultimate goal of esthetic, immediate tooth replacement therapy (EITRT).
For immediately placed implants, both the preservation and augmentation of hard and soft tissues are critical factors. Because dimensions of the facial bone around anterior teeth are deemed thin (<1 mm) in most cases,1 measures to preserve this bone, such as flapless therapy, should be considered. Even with caution taken, however, this bone often resorbs, and clinicians must take this into account.2 This involves countering the physiologic negative changes that occur following extraction. The loss of height and width of the facial bone crest and volume of alveolus need to be factored in when performing EITRT. This augmentation-based concept has demonstrated significant but not complete ridge preservation.3 Grafting the buccal "gap" associated with immediate implants has been demonstrated to preserve equal buccal-palatal ridge dimensions when compared to grafting sockets prior to implant placement.4 Additional steps, such as soft-tissue augmentation either with soft-tissue autograft or allograft combined with bone grafting5,6 or dual-zone bone grafting,7 have shown to preserve ridge dimensions and increase peri-implant mucosal thickness. The author has demonstrated that combining dual-zone bone grafting with a dermal allograft (ie, Dermal Apron Technique® [term trademarked by the author]) (Figure 1) can result in soft-tissue thickness comparable to autogenous soft-tissue grafts.6
Currently, immediate implant placement in the esthetic zone is performed with a palatal bias (Figure 2).7 Angulation of the implant within the extraction socket favoring a larger buccal gap space has been shown to increase soft-tissue dimensions of the peri-implant mucosa.8,9 With natural healing, it has been demonstrated that the volume of bone between the implant and socket wall is not maintained to the degree that grafting achieves.10 Respecting the biologic principles of immediate implant placement and the importance of incorporating an augmentation approach, the angulation of the implant can impact the esthetic outcome in significant ways. The anatomic constraints of the premaxilla often necessitate immediate implant placement with a palatal bias and a significant facial angulation, requiring custom abutments and cement retention.11,12 The platform of these implants, therefore, is in closer proximity to the facial bone, reducing the gap space available for grafting. This also results in pressure against the facial soft tissue because of the angled abutments, precipitating soft-tissue recession.13 Tapered implants, which are geared toward increasing primary stability, are at their widest at the implant platform, so distances between the implant and facial osseous crest and adjacent teeth or implants are decreased.
Novel Implant Designs
In recent years, novel implant designs have been aimed at improving clinical outcomes. An implant with a built-in angle correction at the platform level not only can increase the probability of the use of screw retention but also reduce pressure placed on the submucosa, decreasing risk of recession. This subcrestal angle correction (SAC) implant design has proven to maintain marginal bone, soft tissue, and stability levels at 5 years of follow-up.14 Additionally, the angle correction provided by the implant decreases the risk of abutment screw loosening compared to straight abutment screws when loaded in an off-axis manner.15
A by-product of the SAC implant design is greater distance facially between the abutment connection, or microgap, and the implant platform. This is known as a variable platform switch (VPS). This greater offset compared to traditional platform-switched connections has demonstrated increased soft-tissue thickness versus uniaxial implants for EITRT.16
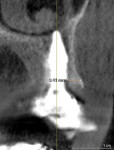
Achieving primary implant stability at the time of EITRT facilitates immediate temporization. As previously mentioned, tapered implants are often used instead of parallel-walled implants because of their ability to achieve a higher insertion torque and/or implant stability quotient (ISQ).17 Unfortunately, tapered implants are widest at the platform, complicating biologic considerations. Recently, a novel, inverted body design implant has addressed the issues of achieving adequate primary stability and increasing implant-tooth or implant-implant distances, as well as reducing proximity to the facial socket wall and increasing gap space.18,19 This implant has demonstrated the ability to achieve high levels of insertion torque, enable enhancement of thin facial bone, increase distances between the implant and adjacent teeth, and facilitate screw retention for temporary and definitive prostheses.20 In a 1-year multicenter study, this type of implant exhibited stable ridge contours, facial bone measurements of 1.5 mm to 2 mm thickness (Figure 3), and soft-tissue thickness of 3 mm when combined with a SAC implant design and dual-zone bone grafting for EITRT.21
Contemporary EITRT requires surgeons to consider the long-term outcomes and how to maximize results by following the aforementioned principles. The author recommends utilizing implants that predictably achieve primary stability, respect adequate distance from facial and proximal anatomic structures, and provide opportunities for augmentation and screw retention.
Restorative Considerations
Restorative factors, such as proper sub- and supragingival abutment/crown contours,22 physiologically favorable contact areas, and occlusal schemes, are just as critical to success as surgical factors and must be considered when fabricating temporary restorations at the time of EITRT (Figure 4). Producing smooth, under-contoured or adequately contoured subgingival provisional restorations will reduce the incidence of mucosal recession and inflammation.23 In most EITRT cases, the temporary crown will have no occlusal contact with teeth in the opposing arch. However, final restorations are typically placed into function and require meticulous occlusal management to avoid excessive forces, which are frequently associated with abutment screw loosening or fracture. Also, the use of screw retention obviates the need for cement, which is often associated with peri-implant inflammation and peri-implantitis.
A recent study by the present author and colleagues focused on the soft-tissue thickness surrounding implants implemented in EITRT.24 When comparing uniaxial implants to tapered SAC and inverted body design SAC implants, both of the latter types, engineered with subcrestal angle corrections and VPS, achieved more than 3.70 mm soft-tissue thickness, while the uniaxial implants achieved an average of 2.74 mm thickness. Importantly, all 46 implants in this three-part comparative study were placed into maxillary anterior sites (canine-to-canine) with identical augmentation procedures (Dermal Apron Technique). The only variable found to exert a significant effect on mucosal thickness was the implant platform. The two cohorts receiving SAC/VPS implants achieved identical and robust soft-tissue thickness. The same authors also found a correlation between the insertion torque of these inverted body design implants and the ISQ values, whereas this was not the case with parallel-walled implants in identical extraction sites.25,26 By increasing the primary stability of immediately placed implants and soft-tissue thickness, short- and long-term parameters of successful therapy are often achieved.
Conclusion
Successful EITRT depends on multiple factors ranging from implant selection, positioning, and design, to augmentation and temporization methods. Newer implant designs can achieve higher primary stability and increase opportunities for screw retention. Less-invasive grafting techniques reduce morbidity without compromising esthetics and bone maintenance. Proper physiologic contours of provisional restorations enhance esthetics and increase soft-tissue dimensions. While these are not the only factors to consider, they play especially critical roles in attaining optimal outcomes.
REFERENCES
1. Huynh-Ba G, Pjetursson BE, Sanz M, et al. Analysis of the socket wall dimensions in the upper maxilla in relation to immediate implant placement. Clin Oral Implant Res. 2010;21(1):37-42.
2. Chen ST, Darby I. The relationship between facial bone wall defects and dimensional alterations of the ridge following flapless tooth extraction in the anterior maxilla. Clin Oral Implants Res. 2017;28(8):931-937.
3. Roe P, Kan JYK, Rungcharassaeng K, et al. Horizontal and vertical dimensional changes of peri-implant facial bone following immediate placement and provisionalization of maxillary anterior single implants: a 1-year cone beam computed tomography study. Int J Oral Maxillofac Implants. 2012;27(2):393-400.
4. Cardaropoli D, Bellomo M, Tamagnone L, Leonardi R. Bone and soft tissue modifications in immediate implants versus delayed implants inserted following alveolar ridge preservation: a randomized controlled clinical trial. Part II: radiographic outcomes. Int J Periodontics Restorative Dent. 2022;42(4):487-494.
5. Yoshino S, Kan JYK, Rungcharassaeng K, et al. Effects of connective tissue grafting on the facial gingival level following single immediate implant placement and provisionalization in the esthetic zone: a 1-year randomized controlled prospective study. Int J Oral Maxillofac Implants. 2014;29(2):432-440.
6. Levin BP, Chu SJ. Changes in peri-implant soft tissue thickness with bone grafting and dermis allograft: a case series of 15 consecutive patients. Int J Periodontics Restorative Dent. 2018;38(5):719-727.
7. Chu SJ, Salama MA, Salama H, et al. The dual-zone therapeutic concept of managing immediate implant placement and provisional restoration in anterior extraction sockets. Compend Contin Educ Dent. 2012;33(7):524-534.
8. Le BT, Borzabadi-Farahani A, Pluemsakunthai W. Is buccolingual angulation of maxillary anterior implants associated with the crestal labial soft tissue thickness? Int J Oral Maxillofac Surg. 2014;43(7):874-878.
9. Pluemsakunthai W, Le B, Kasugai S. Effect of buccal gap distance on alveolar ridge alteration after immediate implant placement: a microcomputed tomographic and morphometric analysis in dogs. Implant Dent. 2015;24(1):70-76.
10. Tarnow DP, Chu SJ, Salama MA, et al. Flapless postextraction socket implant placement in the esthetic zone: part 1. The effect of bone grafting and/or provisional restoration on facial-palatal ridge dimensional change - a retrospective cohort study. Int J Periodontics Restorative Dent. 2014;34(3):323-331.
11. Sung CE, Cochran DL, Chen WC, et al. Preoperative assessment of labial bone perforation for virtual immediate implant surgery in the maxillary esthetic zone. A computer simulation study. J Am Dent Assoc. 2015;146(11):808-819.
12. Gonzalez-Martin O, Veltri M. Immediate implant in maxillary central incisors and prosthetic screw channel: a CBCT feasibility study. Int J Periodontics Restorative Dent. 2012;41(2):245-251.
13. Su H, Gonzalez-Martin O, Weisgold A, Lee E. Considerations of implant abutment and crown contour: critical contour and subcritical contour. Int J Periodontics Restorative Dent. 2010;30(4):335-343.
14. Ma S, Tawse-Smith A, Brown SDK, Duncan W. Immediately restored single implants in the aesthetic zone of the maxilla using a novel design: 5-year results from a prospective single-arm clinical trial. Clin Implant Dent Relat Res. 2019;21(2):344-351.
15. Hotinski E, Dudley J. Abutment screw loosening in angulation-correcting implants: an in vitro study. J Prosthet Dent. 2019;121(1):151-155.
16. Levin BP, Saito H, Reynolds MA, Chu SJ. Changes in peri-implant soft tissue thickness with bone grafting and dermis allograft. Part II: a comparative retrospective case series using a subcrestal angle correction implant design. Int J Periodontics Restorative Dent. 2020;40(4):539-547.
17. Freitas AC Jr, Bonfante EA, Giro G, et al. The effect of implant design on insertion torque and immediate micromotion. Clin Oral Implants Res. 2012;23(1):113-118.
18. Nevins M, Chu SJ, Jang W, Kim DM. Evaluation of an innovative hybrid macrogeometry dental implant in immediate extraction sockets: a histomorphometric pilot study in foxhound dogs. Int J Periodontics Restorative Dent. 2019;39(1):29-37.
19. Chu SJ, Ostman PO, Nicolopoulos C, et al. Prospective multicenter clinical cohort study of a novel macro hybrid implant in maxillary anterior postextraction sockets: 1-year results. Int J Periodontics Restorative Dent. 2018;38(suppl):s17-s27.
20. Chu SJ, Levin BP, Egbert N, et al. Use of a novel implant with an inverted body-shift and prosthetic angle correction design for immediate tooth replacement in the esthetic zone: a clinical case series. Int J Periodontics Restorative Dent. 2012:41(2):195-204.
21. Chu SJ, Saito H, Levin BP, et al. Outcomes of a 1-year prospective single-arm cohort study using a novel macro-hybrid implant design in extraction sockets: Part 1. Int J Periodontics Restorative Dent. 2021;41(4):499-508.
22. Schoenbaum TR, Klokkevold PR, Chang YY. Immediate implant-supported provisional restoration with a root-form pontic for the replacement of two adjacent anterior maxillary teeth: a clinical report. J Prosthet Dent. 2013;109(5):277-282.
23. Schoenbaum TR, Chang YY, Klokkevold PR, Snowden JS. Abutment emergence modification for immediate implant provisional restorations. J Esthet Restor Dent. 2013;25(2):103-107.
24. Levin BP, Saito H, Chu S, et al. Changes in peri-implant soft tissue thickness with bone grafting and dermis allograft. Part III: a case series using a novel, hybrid implant design with a subcrestal angle correction. Int J Periodontics Restorative Dent. 2022;42(6):723-729.
25. Levin BP, Chu SJ, Saito H, et al. A novel implant design for immediate extraction sites: determining primary stability. Int J Periodontics Restorative Dent. 2021;41(3):357-364.
26. Levin BP. The correlation between immediate implant insertion torque and implant stability quotient. Int J Periodontics Restorative Dent. 2016;36(6):833-840.
ABOUT THE AUTHOR
Barry P. Levin, DMD
Clinical Associate Professor, Department of Graduate Periodontology, University of Pennsylvania School of Dental Medicine, Philadelphia, Pennsylvania; Private Practice limited to Periodontics and Implant Dentistry, Jenkintown, Pennsylvania; Diplomate, American Board of Periodontology