Coronectomy: An Alternative to Complicated Full-Bony Impacted Tooth Removal
Gary Orentlicher, DMD; and Andrew Horowitz, DMD, MD
Abstract: The removal of impacted teeth is a common office-based oral and maxillofacial surgical procedure. Complications associated with the procedure are uncommon; however, in the mandible, close proximity of the third molars to the inferior alveolar nerve can potentially lead to temporary or permanent sensory disturbances. The intentional partial odontectomy (coronectomy) procedure is a surgical option aimed at mitigating and reducing the incidence of this potential risk and complication.
In patient cases in which an impacted tooth, typically a third molar, is in close proximity to the inferior alveolar nerve (IAN) canal, the intentional partial odontectomy (coronectomy) procedure has become a surgical treatment option used to avoid nerve injury. The effectiveness of the procedure in reducing the incidence of IAN sensory disturbances has been described frequently in the literature.1,2
IAN injury is a well-known potential risk and complication of the removal of impacted third molars. The risk of IAN injury has been reported as ranging from 0.5% to 8%, with an incidence of permanent injury reported as less than 1%.3-7 Preoperative patient evaluations are commonly made using conventional 2-dimensional (2D) periapical and panoramic radiographs. An increased risk of nerve injury is possible in patient cases in which various radiographic signs show a close relationship between mandibular third molars and the IAN canal.8 These signs include an IAN canal appearing to cross over the tooth roots, diversion and/or narrowing of the IAN canal, interruption of the "white" superior cortical aspect of the IAN canal, and deflection, darkening, or bifid root apex findings. With today's availability of cone-beam computed tomography (CBCT), it is strongly recommended that for patients who exhibit any of these signs, additional 3-dimensional (3D) radiographic evaluations be carried out prior to surgery.
Case reports describing the use of coronectomy to mitigate potential IAN injury were first published in the early 1990s.9,10 Publications in the 2000s that outlined successful procedure outcomes have led to its more common use.1,2
The Coronectomy Procedure
The procedure typically involves removing the entire crown of the tooth, including all the enamel, while intentionally leaving the root portion of the tooth that is close to the IAN canal. A conventional buccal hockey stick incision is made, followed by elevation of a full-thickness mucoperiosteal flap. Using a fissure bur, the crown of the tooth is exposed with conservative bone removal. A fissure bur is then utilized at a 30-degree angle to section the crown from the roots. A round bur is then used to reduce the root portion of the tooth to a point 3 mm to 4 mm below the bone crest in all dimensions, with care taken to remove all enamel. The vital exposed pulp does not require endodontic treatment.
Decayed third molars with possible pulpal exposures are not candidates for coronectomies. If mobility of the root fragment(s) is noted at surgery, it is advisable to remove the mobile root(s) completely. The area is then irrigated with sterile solution and closed primarily in a watertight fashion. Postoperative instructions and medications are given to the patient, similar to those used for the removal of an impacted third molar.
Although occurring less frequently than those encountered with complete impacted third molar removal, common reported postoperative sequelae of a coronectomy include pain, swelling, infection, alveolar osteitis ("dry socket"), and mild neurosensory deficit.1,11-14 The most common postoperative finding reported is the potential for root migration and exposure. The reported incidence of root migration ranges from 13% to 97%,15-17 occurring primarily during the first postoperative year.11,13 While root migration is a common finding radiographically, it rarely requires surgical intervention unless it progresses to intraoral exposure and pain, inflammation, and/or infection. If this occurs, because the root migration is usually in a direction in which the roots move superiorly, away from the IAN canal and toward the ridge crest, their removal is typically a simple surgical procedure. Nerve injury has not been a reported complication of secondary root removal. There is, however, a recent case report of a neurologic deficit occurring 9 months after a coronectomy that was due to root migration of a curved/hooked root intentionally left in place surrounding the IAN canal. The neurologic deficit resolved after secondary root removal.18 A decrease in root migration has been reported when guided bone regeneration techniques are used with coronectomy surgery.19
The following case presentations describe coronectomy procedures performed in patients requiring the removal of impacted third molars.
Case Presentations
Case 1
A 17-year-old female patient presented with a complaint of pain and pressure in her mandibular third molar areas. The patient's past medical history was negative, she took no medications, and she had no known allergies.
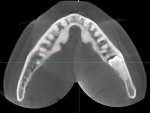
A panoramic radiograph was taken, which revealed full-bony impacted teeth Nos. 1, 16, 17, and 32. Teeth Nos. 17 and 32 appeared to be positioned in close proximity to the IAN canal with a radiographic loss of the IAN canal density and a darkening of the apical aspect of the roots. A CBCT scan then revealed an intimate contact between the roots and the IAN canal. A digital imaging and communications in medicine (DICOM) dataset was created and imported into the implant software (DTX Studio™, NobelBiocare/Envista Holdings Corp., dtxstudio.com) to create 3D reformation images.
The patient was administered intravenous (IV) sedation and local anesthesia, and teeth Nos. 1 and 16 were removed and coronectomy procedures were performed on teeth Nos. 17 and 32. The patient's postoperative course was uneventful, and no sensory disturbances were reported. (See Figure 1 through Figure 8.)
Case 2
A 20-year-old male patient presented with a complaint of pain, pressure, and swelling in his mandibular third molar areas. His past medical history was negative, he took no medications, and he had no known allergies.
A panoramic radiograph was taken, which revealed full-bony impacted teeth Nos. 1, 16, 17, and 32. Teeth Nos. 17 and 32 appeared to be positioned in close proximity to the IAN canal with a radiographic loss of the IAN canal density and a darkening of the apical aspect of the roots. Additionally, the IAN canal associated with tooth No. 32 appeared to be displaced inferiorly. A CBCT scan was taken, which revealed an intimate contact between the roots and the IAN canal. A DICOM dataset was created and imported into the implant software (DTX Studio) to create 3D reformation images.
With the patient under IV sedation and local anesthesia, teeth Nos. 1 and 16 were removed and coronectomy procedures were performed on teeth Nos. 17 and 32. As in the first case, the patient's postoperative course was uneventful, and no sensory disturbances were reported. (See Figure 9 through Figure 12.)
Case 3
The patient, an 18-year-old woman, presented with a complaint of pain and pressure in her mandibular third molar areas. Her past medical history was negative, she took no medications, and she had no known allergies.
A panoramic radiograph revealed full-bony impacted teeth Nos. 1, 16, 17, and 32. Teeth Nos. 17 and 32 appeared to be positioned in close proximity to the IAN canal with a radiographic loss of the IAN canal density and a darkening of the apical aspect of the roots. Additionally, the IAN canal associated with tooth No. 32 appeared to be displaced inferiorly. A CBCT scan was taken, which revealed an intimate contact between the roots and the IAN canal. A DICOM dataset was created and imported into the implant software (DTX Studio) to create 3D reformation images.
The patient was administered IV sedation and local anesthesia, and teeth Nos. 1 and 16 were removed and coronectomy procedures were performed on teeth Nos. 17 and 32. As in the first two cases, the patient's postoperative course was uneventful, and no sensory disturbances were reported. (See Figure 13 through Figure 16.)
Case 4
A 33-year-old male patient presented with a complaint of pain, pressure, and chronic infection in his mandibular left third molar area. He was evaluated by a local periodontist who took a CBCT scan, which revealed a deeply horizontally impacted tooth No. 17 with a horizontally impacted supernumerary tooth No. 67 superior to and on top of No. 17. Significant bone loss was obvious radiographically, distal and buccal to the apex of tooth No. 18, which was confirmed by periodontal probing. His past medical history was negative, he took no medications, and had no known allergies.
The patient was referred to the authors' office for an evaluation and treatment. In addition to the above radiographic findings, review of the CBCT scan revealed tooth No. 17 positioned in close proximity to the IAN canal with a radiographic loss of the IAN canal density in relation to the roots of the tooth. Under IV sedation and local anesthesia, teeth Nos. 16 and 18 and supernumerary teeth Nos. 66 and 67 were removed, and a coronectomy was performed on deeply impacted tooth No. 17. A mineralized bank bone graft was placed in the region of tooth No. 18 to prepare the site for a future implant placement. The patient's postoperative course was uneventful, and no sensory disturbances were reported. (See Figure 17 through Figure 24.)
Conclusion
In patient cases requiring the removal of an impacted tooth, with 2-dimensional and 3-dimensional evidence of a close relationship between the root(s) of the tooth and the inferior alveolar nerve canal, coronectomy is a well-documented option to successfully mitigate the risk and sequelae of nerve trauma.
About the Authors
Gary Orentlicher, DMD
Section Chief, Oral and Maxillofacial Surgery, White Plains Hospital, White Plains, New York; Private Practice in Oral, Maxillofacial, and Implant Surgery, Scarsdale, New York; Diplomate, American Board of Oral and Maxillofacial Surgery
Andrew Horowitz, DMD, MD
Associate Attending, White Plains Hospital, White Plains, New York; Private Practice in Oral, Maxillofacial, and Implant Surgery, Scarsdale, New York; Fellow, American College of Surgeons
References
1. Renton T, Hankins M, Sproate C, McGurk M. A randomised controlled clinical trial to compare the incidence of injury to the inferior alveolar nerve as a result of coronectomy and removal of mandibular third molars. Br J Oral Maxillofac Surg. 2005;43(1):7-12.
2. Pogrel MA, Lee JS, Muff DF. Coronectomy: a technique to protect the inferior alveolar nerve. J Oral Maxillofac Surg. 2004;62(12):1447-1452.
3. Valmaseda-Castellon E, Berini-Aytes L, Gay-Escoda C. Inferior alveolar nerve damage after lower third molar surgical extraction: a prospective study of 1117 surgical extractions. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;92(4):377-383.
4. Sarikov R, Juodzbalys G. Inferior alveolar nerve injury after mandibular third molar extraction: a literature review. J Oral Maxillofac Res. 2014;5(4):e1.
5. Kipp DP, Goldstein BH, Weiss WW Jr. Dysesthesia after mandibular third molar surgery: a retrospective study and analysis of 1,377 surgical procedures. J Am Dent Assoc. 1980;100(2):185-192.
6. Wofford DT, Miller RI. Prospective study of dysesthesia following odontectomy of impacted mandibular third molars. J Oral Maxillofac Surg. 1987;45(1):15-19.
7. Osborn TP, Fredrickson G Jr, Small IA, Torgerson TS. A prospective study of complications related to mandibular third molar surgery. J Oral Maxillofac Surg. 1985;43(10):767-769.
8. Rood JP, Shehab BA. The radiological prediction of inferior alveolar nerve injury during third molar surgery. Br J Oral Maxillofac Surg. 1990;28(1):20-25.
9. Zola MB. Avoiding anesthesia by root retention. J Oral Maxillofac Surg. 1993;51(8):954.
10. Freedman GL. Intentional partial odontectomy: report of a case. J Oral Maxillofac Surg. 1992;50(4):419-421.
11. Pedersen MH, Bak J, Matzen LH, et al. Coronectomy of mandibular third molars: a clinical and radiological study of 231 cases with a mean follow-up period of 5.7 years. Int J Oral Maxillofac Surg. 2018;47(12):1596-1603.
12. Monaco G, De Santis G, Pulpito G, et al. What are the types and frequencies of complications associated with mandibular third molar coronectomy? A follow-up study. J Oral Maxillofac Surg. 2015;73(7):1246-1253.
13. Leung YY, Cheung LK. Safety of coronectomy versus excision of wisdom teeth: a randomized controlled trial. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108(6):821-827.
14. Monaco G, De Santis G, Gatto MR, et al. Coronectomy: a surgical option for impacted third molars in close proximity to the inferior alveolar nerve. J Am Dent Assoc. 2012;143(4):363-369.
15. Pedersen MH, Matzen LH, Hermann L, Nørholt SE. Migration of the root complex after coronectomy occurs within the first year after surgery: a 5-year radiographic analysis and protocol suggestion. Oral Surg Oral Med Oral Pathol Oral Radiol. 2019;128(4):357-365.
16. Leung YY, Cheung KY. Root migration pattern after third molar coronectomy: a long-term analysis. Int J Oral Maxillofac Surg. 2018;47(6):802-808.
17. Cheung KY, Leung YY. Long-term analysis of root migration after third molar coronectomy. Int J Oral Maxillofac Surg. 2017;46(suppl 1):106.
18. Steinberg MJ, Nick MJ. Displacement of the inferior alveolar bundle secondary to post coronectomy root migration: a case report. J Oral Maxillofac Surg. 2021;79(9):1837-1841.
19. Leung YY. Guided bone regeneration to reduce root migration after coronectomy of lower third molar: a randomized clinical trial. Clin Oral Investig. 2019;23(4):1595-1604.