From Conventional to Complex Treatments, Digital Technologies Are Simplifying Implant Dentistry
Gary Orentlicher, DMD
In the past decade, the shifting of dentistry into the digital world has become obvious to any dentist or dental specialist. Many restorative dentists now consider themselves "digital dentists," performing all their crown and bridge restorative planning and fabrication in a digital environment. In preparation for this article, the author asked both a prosthodontist and the owner of a large state-of-the-art dental laboratory with whom he has worked closely the following questions: "These days, what percentage of your crown and bridge cases are being done fully digital?" Then, "What is the answer to the same question 5 years ago?"
The prosthodontist answered that for crowns and bridges (with some exceptions for bridges), including implants (but not full arches), "close to 100%" of cases are now fully digital, while "maybe 25%" were 5 years ago (personal communication with Jason Sauer, DDS, of Westchester Prosthodontics, White Plains, New York, March 29, 2024). The dental laboratory owner answered, "My lab is different than others. We're about 60% digital, but digital is rapidly increasing. I'd say the majority of labs are 80% to 90% digital. Five years ago, we were 70% to 80% hand (analog.) We went from three mills pre-Covid to 30 different machines post-Covid (printers, mills, and scanners)" (personal communication with Steven Pigliacelli, MDT, of Marotta Dental Studio, Farmingdale, New York, March 29, 2024).
It's fair to say that these comments show that the implementation of digital technologies in dentistry has been dramatic and will continue to expand.
Revolutionizing Implant Treatment
Cone-beam computerized or volumetric technology (CBCT/CBVT) has revolutionized the way dentists/prosthodontists, periodontists, and oral and maxillofacial surgeons evaluate the maxillary and mandibular arches for the placement of dental implants. As always, in patient treatment the goal of improving outcomes and minimizing morbidity and complications is paramount. CBCT is a relatively low-radiation, office-based, small-footprint imaging option that quickly allows the clinician to evaluate the dental arches and the surrounding anatomy in three dimensions (3D). Digital imaging and communication in medicine (DICOM) datasets can be created from CBCT data to allow the data to be imported into third-party software for 3D evaluations and "virtual" treatment planning. Accurate, predictable, digitally directed placement of dental implants can then be accomplished using surgical "static" guides, navigation, or robotic equipment and instrumentation.
For partially edentulous treatment planning and implant placement, standard triangulation language (STL) files from intraoral optical scanners or laboratory model scanners can be imported into third-party treatment planning software, which can overlay the STL dataset(s) over a DICOM dataset from a patient's CT/CBCT scan(s), termed "conversion." This allows for accuracy in importing tooth morphology and soft-tissue anatomy information for treatment planning and guided implant placement. STL files of planned restorations, created digitally or by hand, can be imported as well. Some software enables the end-user (ie, the clinician) to import these DICOM and STL datasets, "convert" or combine the data, and design and add "virtual teeth" for treatment planning. Once virtual treatment planning is complete, the plan can be exported to have a "static" surgical guide fabricated or exported into navigation or robotic guided implant placement software/equipment.
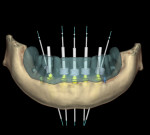
The fully edentulous case workup first usually requires the fabrication of an idealized, well-fitting denture made of hard acrylic (no metal and no barium). The denture will have ideal tooth morphology, anterior-posterior and vertical positioning, tongue space, phonetics, thickness, and occlusion. This denture can be fabricated in an analog or digital environment. An existing denture can be used if it is hard relined and well-fitting. Radiopaque fiducial markers (eg, gutta-percha or small stick-on markers) are then applied to the denture. A bite registration, separating the teeth approximately 3 mm to 4 mm, should always be made between the denture and the dentition in the opposing arch. Fully edentulous digital surgical planning generally requires the use of the double scan technique. The first scan is of the patient wearing the denture with fiducial markers and the bite registration, and gently biting into his or her occlusion. The second scan is a scan of the denture and fiducial markers alone (no bite registration). These two DICOM datasets are then imported into software. The software uses the fiducial marker positions to triangulate and combine the two datasets for treatment planning. Patients with a terminal dentition who require removal of their existing teeth and full-arch implant-supported restorations can be planned similarly using a multiple-piece radiographic guide and the double scan technique for creation of the two aforementioned datasets. These datasets can then similarly be imported into third-party software and used in treatment planning as described above (Figure 1).
Solutions for Severe Atrophy
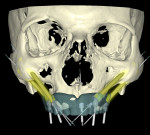
Severely atrophic patient cases present a host of complicated planning and treatment problems prosthetically and surgically. Digital evaluation and treatment planning, regardless of whether the dental implants are planned to be placed guided or nonguided, are strongly recommended. Following the aforementioned patient workup, dataset acquisition, and software importation protocols allows the surgeon to evaluate the patient's hard- and soft-tissue anatomy as it relates to the patient's unique prosthodontic needs and plan. The optimal, least invasive, most predictable treatment plan for a specific complicated patient case can then be planned. Evaluating the bone volume in all areas of the maxilla, mandible, and zygomas is possible. Treatment planning patient cases using tilted implants placed in unusual locations and directions is possible, fully guided.
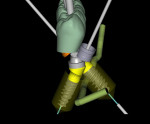
These implants can then be planned to be corrected with angled multi-unit abutments based on the ideal dental restoration and the individual case restorative needs. Implants can be planned for placement in the anterior nasal spine, nasal floor, piriform rim, tuberosity, trans-sinus, pterygoid, or zygoma. Some systems allow for virtual planning of zygomatic implants (Figure 2). Fully guided placement of zygomatic implants is not possible from most manufacturers.
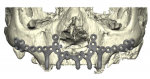
One notable recently introduced system (IPS Implants® Preprosthetic, KLS Martin Group, klsmartin.com) is an innovative, digitally driven, full-arch, non-endosseous implant solution for the prosthodontic and surgical treatment of severe atrophy or large defects of the maxilla or mandible. The technique involves the digital custom design and surgical placement of a full-arch subperiosteal implant, rigidly secured to the maxilla or mandible with multiple titanium screws similar to those used in orthognathic surgery or jaw fracture treatments. The full-arch implant does not require osseointegration. Milled into the full-arch bone plate are four or more parallel vertical "pillars" with standard multi-unit attachments. The pillars are virtually positioned based on the planned restoration in the arch (Figure 3). A provisional restoration is fabricated prior to the surgery and inserted at the time of implant placement and stabilization.
The Power of Technology
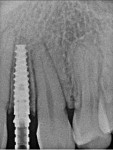
Digitally directed surgical planning and placement can be performed accurately and predictably in single-tooth (Figure 4 through Figure 6), multiple-unit (Figure 7), full-arch, or severely atrophic dental implant patient cases. The power of these technologies has changed the way clinicians plan, visualize, surgically place, and restore conventional and complicated patient treatments.
About the Author
Gary Orentlicher, DMD
Section Chief, Oral and Maxillofacial Surgery, White Plains Hospital, White Plains, New York; Attending Oral and Maxillofacial Surgeon, Manhattan Veterans Administration Hospital, New York, New York; Private Practice, New York Oral, Maxillofacial, and Implant Surgery, Scarsdale, New York; Diplomate, American Board of Oral and Maxillofacial Surgery