Effectiveness of Antibiotics to Reduce Early Implant Loss in Systemically Healthy Patients
Gary Greenstein, DDS, MS; and Dennis Tarnow, DDS
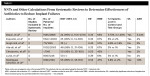
Surprisingly the topic of pre-medication or post-medication with antibiotics related to implant dentistry remains controversial. It would seem that sufficient research data exists to allow clinicians to determine a reasonable recommendation with respect to the use of an antibiotic when placing a dental implant in a systemically healthy patient who is not receiving a bone graft. The literature is replete with narrative assessments1-5 and systematic reviews addressing this subject (Table 1).6-12 However, a number of issues continue to cause confusion regarding the efficacy of drug administration. These include different methodologies employed in studies (eg, dosing regimens), bias in many articles related to subject selection, poor randomization of patients with respect to providing therapies, failure to properly blind examiners, and heterogeneity of studies included in systematic reviews.11 Furthermore, various pitfalls that are common in statistical assessments (eg, interpreting clinical significance) must be taken into account when evaluating therapeutic benefits of antibiotics.13,14
Some systematic reviews have noted that when test groups receiving antibiotics were compared to placebo groups with respect to implant loss, the percentage of early implant failures was not statistically significantly reduced if antibiotics were administered.8,11 The authors of these reviews concluded that dentists should refrain from using antibiotics prophylactically in healthy individuals when the risk of developing an infection is unlikely. In contrast, other systematic reviews demonstrated that there are statistically significantly fewer implants lost when antibiotics are administered in conjunction with implantations.6,7,9,10,12 Sometimes no statistically significant differences were found between test and control groups, but measures such as number needed to treat (NNT) demonstrate a benefit when prescribing an antibiotic as an adjunct to implant placement.8,11
Reaching a clear consensus regarding the ability of antibiotics to reduce implant loss is complicated by the fact that quantitatively (numerically or percentages) improvements are small when test and control groups are compared (Table 1).6-12 Consequently, the clinical significance of benefits provided by antibiotics is open to interpretation. Nevertheless, even if there is conflicting data, the preponderance of information if scrutinized carefully should be able to provide reasonable guidance to protect patients from unnecessary implant loss and avoid antibiotic overuse that results in proliferation of antibiotic-resistant bacterial strains.1,15-17 The present authors, therefore, evaluated the literature from a clinician's perspective to determine if there is a biologically plausible basis for antibiotic use when placing dental implants, and to select the most appropriate dosing regimen for systemically healthy patients who are not undergoing adjunctive procedures such as bone grafting.
Statistical Techniques Frequently Used to Assess Data
This assessment of the literature focuses on data derived from seven recent systematic reviews (2013-2019) that provided statistical assessments and NNT values with respect to the utility of antibiotics to reduce early implant loss.6-12Many of the clinical trials included in these systematic reviews overlap among the articles. An advantage of systematic reviews compared to single studies or narrative analyses pertains to their search strategy. Systematic reviews employ inclusion and exclusion criteria to facilitate selection of clinical trials with less bias before subjecting them to group analysis. Systematic reviews frequently include a meta-analysis, which is a statistical technique that combines data from different studies into a single approximation of effect size.18
To help understand published data, a review of issues related to statistical techniques and clinical significance is necessary. Statistical significance testing provides a "yes" or "no" answer as to whether there are differences between variables in test and control groups. The finding that there is a statistically significant difference between groups, however, only denotes that the dissimilarity did not occur by chance.19,20 It does not connote that the variation between groups is large or important. Therefore, clinicians need to determine if they think a statistically significant finding is clinically significant. The definition of clinical significance, however, varies depending on the specific clinical field being addressed, the size of the effect, the measurement used to evaluate a therapy, and the clinical importance of the findings.21 Accordingly, it has been suggested that clinical significance denotes a change that may alter how a clinician will treat a patient and this value judgment varies depending on the situation.20,21
In healthcare, risk refers to the probability of a bad outcome.13 Different terms such as absolute risk reduction (ARR), relative risk (RR), and relative risk reduction (RRR) are used to characterize the effect size of an intervention. Formulas for these definitions are listed in Table 2.22
Another calculation that can help clinicians understand the clinical significance of data is the NNT.23,24 The NNT is often used in the medical literature to demonstrate the number of individuals (or sites) who must be treated with an intervention therapy in order to prevent one additional adverse event compared to the expected results in the control group. The NNT is the inverse of the difference between the proportion of events in the control group (Pc) and the proportion of events in the intervention group (Pi): NNT = 1/(Pc-Pi).25 For example, if two groups of patients are compared with respect to implant loss, and the control group (Pc) receives no antibiotics and the intervention group (Pi) is given amoxicillin, and subsequently 6% of the patients in the control group lose an implant and 2% of the patients in the intervention group lose an implant, then the NNT would be calculated as: NNT = 1/.06-.02 = 25.7 This means that 25 individuals must be treated with a prophylactic antibiotic to avoid loss of an implant in another patient.
NNT values were used in the present analysis to provide a clinically relevant parameter to assess studies where statistical significance testing does not clarify the clinical significance of the use of antibiotics with implant placement. The point of using NNT values was to demonstrate the clinical utility of antibiotic usage with a parameter that can be used to address clinical significance.
Antibiotics Regimen in a Healthy Patient Prior to Dental Implantation
Antibiotics are used to therapeutically treat dental infections and as adjuncts to conventional therapy in a prophylactic manner. Prophylactic use of an antibiotic with dental implants means that it is being administered before, during, or after surgery to prevent infectious complications.6,8,26,27 Originally, Brånemark et al suggested that patients receiving dental implants should be administered phenoxymethypenicillin 1 hour before the procedure and for an additional 10 days to enhance early implant survival.28Contemporaneously, the need for prophylactic adjunctive antibiotics with implants has been questioned.3,5,8,11
Data From Seven Current Systematic Reviews
Seven systematic reviews were summarized with respect to the ability of adjunctive antibiotic therapy to reduce early implant loss. In Table 1, the reviews, which span from 2013 to 2019, are listed in order of increasing NNT values.6-12 Five systematic reviews found that antibiotic administration (test groups) in conjunction with implant placement statistically significantly reduced implant loss when compared to placebo groups that received no antibiotics.6,7,9,10,12 Two other reviews found no statistically significant difference between test and control groups with respect to reducing implant failures.8,11
In the clinical trials, the percentage of implant loss with (test group) and without (control group) adjunctive antibiotics ranged, respectively, from 1% to 2% and from 3% to 6% (Table 1).6-12 Differences between control and treatment groups were small. The ARR (ie, the percentage implants failed in control group minus percentage implants lost in test group) varied from 1.8% to 4% (Table 1).6-12 The RRR for losing an implant when antibiotics were given spanned from 45% to 67% (Table 1).6-12 RRR indicates the percentage reduced risk reduction for losing an implant in the test group (antibiotic taken) versus the control group. The NNT values in Table 1 range from 24 to 55. The presented NNTs in Table 1 refer to the number of patients that need to be treated with antibiotics to avoid one more patient with an implant loss.6-12
Resistance and Adverse Reactions to Antibiotics
Currently, dentists prescribe around 10% of common antibiotics,29 and it has been estimated that one in three outpatient prescriptions are unnecessary.30 The World Health Organization states that antibiotics are the most commonly misused medicine, and antimicrobial resistance is becoming widespread and can result in the loss of antibiotic efficacy.16 Antimicrobial resistance is believed to result in 25,000 deaths per year.31 Furthermore, resistant bacterial strains make it more difficult to treat infections, and prescribed antibiotics may need to be administered for extended periods of time to be effective.32 Therefore, a decrease in antibiotic use would result in a reduction of resistant antibiotic bacterial strains and would also lessen adverse events such as gastrointestinal and allergic reactions.33,34 Accordingly, the effects of antibiotics must be evaluated with respect to their benefit versus risk ratio. Previously, guidelines were published with respect to what systemic conditions require premedication with antibiotics prior to dental procedures and this applies to patients receiving dental implants.35,36
Discussion
Implant loss can be attributed to four possible reasons: biological, mechanical, iatrogenic, and functional.37 Also, implant survival rates vary among studies, as there are differences related to the type of implant and its surface, the treating clinician's experience, history of chronic periodontitis, bone quality, smoking status, and implant location.38-40 In addition, antibiotic coverage may statistically significantly affect early implant survival rates.6,7,9,10,12
Transparency is needed with respect to the utility of antibiotics in conjunction with implant placement in systemically healthy patients to reduce the incidence of implant loss. Two major issues need to be addressed. First, there is the question of whether antibiotics administered in conjunction with implant placement decrease implant failures to a level that would be considered clinically significant. Second, if this is true, then what is the best dosing schedule to achieve this outcome?
Clinical trials compared implant loss among groups that did and did not receive adjunctive antibiotic therapy to determine if there was a statistically significant difference between treatment and control groups.6-12 The finding of statistical significance between groups, however, often fails to provide the clinician with clear understanding regarding the clinical benefit of antibiotic therapy. Five of the seven systematic reviews in Table 1 indicated that antibiotics (ie, amoxicillin, penicillins, clindamycin) provided a statistically significant reduction of implant loss when antibiotics were prescribed, but the differences were small between treatment groups and the clinical significance of these findings is unclear.6,7,9,10,12 The other two systematic reviews found no statistically significant differences with respect to reducing implant loss between groups treated with and without antibiotics; however, they did provide other information that may be clinically relevant (ie, NNT calculations).8,11 In this regard, calculations can be made to determine how many patients need to be treated so that another patient does not lose an additional implant. This calculation is referred to as NNT.13,14,24
In general, NNT calculations are easier to understand than other statistical techniques concerning drug benefits, because they can define a useful clinical outcome. NNTs calculated from systematic reviews provide a high level of clinical relevance, because these reviews cover many studies. Nevertheless, systematic reviews need to be of high quality and adequate size and demonstrate validity. In addition, the NNTs should be considered in light of other issues such as cost of therapy, the individual's social and medical priorities, and development of antibiotic-resistant strains. In medicine a NNT of five or lower is desirable. However, there are situations when a NNT of 50 or 100 is considered a desired result. For instance, daily aspirin used to prevent one death 5 weeks after myocardial infarction has a NNT of 40. This is a high NNT but still provides a benefit.41
NNT assessments from systematic reviews regarding the effectiveness of antibiotics are listed in Table 1 and range from 24 to 55.6-12 A NNT of 24 means that 24 patients need to be treated with an antibiotic to avoid an additional patient losing an implant. Similarly, a NNT of 55 signifies that 55 individuals must be administered an antibiotic to circumvent an additional patient losing an implant. These two NNTs, 24 and 55, were selected as examples because they represent the high and low NNTs in Table 1. The NNTs in Table 1 are high and the 95% confidence intervals (CI) are large, indicating there is much variability between included studies.
With respect to dental implants, if the NNT is 24 and a clinician places 100 implants with adjunctive antibiotics, this means that 4.17 patients avoided additional implant failures (100/24 = 4.17) (patients receiving implants/NNT = number of patients that avoided implant loss). For an implant surgeon who places 200 implants per year a NNT of 24 means that 8.34 patients (200/24) avoid implant failure due to adjunctive antibiotic coverage. A NNT of 55 for 200 patients means that 3.64 (200/55) individuals circumvent implant loss. The sample size of 200 was chosen to represent an office that places a considerable amount of implants. Mathematically, it may seem like overtreatment to medicate 200 patients to avoid 3.64 to 8.34 patients from losing an implant; however, from the point of view of a clinician who places 200 implants per year, loss of implants in 3.64 to 8.34 patients per year is problematic. When interpreting NNT values, the clinician also needs to consider the cost of retreatment, time, effort, possible loss of bone, and the patient's disappointment if an additional surgery is needed that could have been avoided if an antibiotic were prescribed.
It should be noted that for this literature assessment, systematic reviews were selected that estimated NNTs regarding the number of patients who had to be treated with an antibiotic to avoid an implant failure in another patient; the reviews did not address what occurs if a patient lost multiple implants. From another perspective, if NNTs were calculated for the number of implants that would need to be lost to prevent one additional implant loss if antibiotics were prescribed, then the problem would be lack of independence among implants within patients. Therefore, the best unit for analysis is the patient.
Overuse of antibiotics is recognized as a dilemma, and promiscuous use of these chemotherapeutic agents needs to be eliminated.1,16,17 Nevertheless, clinicians need to decide on an individual case basis if they think the NNTs recorded in Table 1 provide a clinically significant benefit with respect to reducing implant loss. The present authors interpret the data to indicate that antibiotics in conjunction with dental implantation do provide a clinically significant advantage with respect to reducing implant loss in systemically healthy patients not receiving bone grafts.
The next important question is what antibiotic dose is enough to avoid implant loss. Several systematic reviews compared single preoperative dosing with amoxicillin to other antibiotic regimens.7,12 This was done to determine if a loading dose of amoxicillin was sufficient to reduce implant loss compared to postoperative or a combination of preoperative and postoperative antibiotics. It was reported that a single dosing with amoxicillin when compared to a placebo achieves better results than a placebo with respect to reducing implant failures.7 In their systematic review, Esposito et al7 demonstrated 2 gm27,42-44 and 3 gm45 of amoxicillin 1 hour before the procedure reduces loss of implants better than a placebo. The NNT for prophylactic amoxicillin was 25 (95% CI, 14 to 100), and Esposito et al suggested that a 2 gm prophylactic dose seemed sensible.7 There was no reported advantage for reducing postoperative infections with use of prophylactic amoxicillin.7
Rodríguez Sánchez et alalsonoted that a single-dose amoxicillin given preoperatively is beneficial when compared to postoperative amoxicillin.12 Preoperative doses assessed were 1 gm,46,472 gm,26,27,42,45,48 and 3 gm.45 This was compared to a variety of postoperative regimens and combinations of preoperative and postoperative schedules.26,27,46-48 The results indicated that a single dose preoperatively significantly prevented postoperative loss of implants (RR = 0.50, RRR = 50%), whereas postoperative doses of amoxicillin did not (RR = 0.60, RRR = 40%).12 The NNT for preoperative amoxicillin with respect to preventing a patient from losing an additional implant was 67 (95% CI, 26 to 125).12 It is perplexing that Rodríguez Sánchez et al12 found a NNT of 67 and Esposito et al7 recorded a NNT of 25 with respect to how many patients needed to be treated to avoid an additional patient losing an implant when amoxicillin was administered as a loading dose. This large discrepancy can probably be attributed to inclusion of different studies in their analyses. The general NNT for all antibiotics used in the Rodríguez Sánchez et al review was 55.12
Two additional recent studies not listed in Table 1 are worth mentioning, as they broaden the discussion regarding preoperative prophylactic amoxicillin.49,50 Kashani et al published a large study (not a systematic review) that provides additional support for using a 2 gm amoxicillin loading dose prior to implantation.49 They placed implants in 223 patients who were pre-medicated with 2 gm of amoxicillin and in 224 patients who did not receive any pre-medication. There was a statistically significant reduction in the percentage of patients who experienced implant loss who received 2 gm of amoxicillin when compared to individuals who did not receive antibiotics, 4.9% versus 12.9% respectively. The present authors calculated the NNT values for patients in the Kashani et al study49 and it was 12.5 (NNT = 1/12.9%-4.9% = 12.5).
Romandini et al presented a different point of view in a systematic review addressing antibiotic prophylaxis prior to dental implant placement.50 Their review included nine randomized controlled trials (in some studies other therapies besides implants were conducted) and no NNT values were reported. They compared the rate of early implant loss with respect to an adjunctive placebo (ie, no antibiotic), versus a 2 gm or 3 gm loading dose of amoxicillin 1 hour before implantations. The implant failure rate among patients taking antibiotics versus not taking antibiotics was, respectively, 1.8% versus 5.6%. All protocols with antibiotics obtained a better result than treatment with a placebo. The authors noted that a 3 gm prophylactic dose provided the optimum therapy to reduce early implant loss based on one clinical trial included in their meta-analysis. They also stated that there was inadequate data to confidently advise using this specific dosage (3 gm) and that a 2 gm preload dose did not seem to be an effective preloading dose. This latter comment does not agree with the present authors' interpretation of the data and is included to underscore that the precise ideal loading dose has not been confirmed. Nevertheless, clinicians need to make decisions based on the best available information. In this regard, the present authors interpret the data provided by Esposito et al,7 Rodríguez Sánchez et al,12 and Kashani et al49 to support the concept that 2 gm of amoxicillin 1 hour prior to implantations in a systemically healthy patient seems to help reduce early implant failures.
With respect to pharmaceutical availability and efficacy, it should be noted that evaluations have been done to determine the single-dose bioavailability of amoxicillin in alveolar bone plasma and venous blood. If 1 gm of amoxicillin is administered 1 hour before a procedure, the level of amoxicillin in the bone plasma is 5 ug/ml (range 2.04 ug/ml to 11.18 ug/ml) and in the venous blood it is 4.21 ug/ml (range 1.6 ug/ml to 9.98 ug/ml).51 When 2 gm of amoxicillin were administered 1 hour before surgery the levels of amoxicillin were 18.2 ug/ml in the alveolar plasma52 and 14 ug/ml in the gingival crevicular fluid.53 This level of amoxicillin exceeds the minimum inhibitory concentration (MIC) for bacteria often associated with local oral infections: Porphyromonas gingivalis - MIC <0.25 ug/ml; Bacteroides forsythus - MIC <0.5 ug/ml; and Fusobacterium spp - MIC <0.25 ug/ml.54 In general, antibiotic efficacy is attained in a range two to four times the MIC for a bacterium,55 which is achieved with a loading dose of 1 gm to 2 gm of amoxicillin.
Numerous other issues need to be considered when assessing data concerning the helpfulness of antibiotics to reduce implant loss. For instance, the systematic reviews addressed in this article used implant failure and infections as primary outcomes to assess antibiotic usefulness. Since antibiotics are directed at reducing the incidence of infections, it is puzzling that most studies do not report a decrease postoperatively when antibiotics are administered compared to a placebo, despite benefits noted regarding a reduction of implant losses.6-10,12 This may be because asymptomatic infections can occur and not be identified clinically.37 On the other hand, it could be argued that early implant failure is a multifactorial event and infection is one of several causes of implant failure. Thus, if other factors are not considered, the utility of antibiotics may be overstated.56 Another concern relates to the duration of studies, which can vary. Pertinently, short-term studies may appear to increase the success of antibiotics to reduce failures because a sufficient amount of time may not have been allowed for implant losses to occur.57
Conclusion
Because only a small number of implants are lost after placement when no adjunctive antibiotics are prescribed, it is understandable that the use of adjunctive antibiotics does not always result in a statistically significant improvement with respect to reducing early implant failures. However, all systematic reviews addressed in this article demonstrated fewer implant losses when antibiotics were administered with implant placement. Five of the seven systematic reviews indicated the reduction in implant loss was statistically significant (Table 1). In addition, NNT calculations provide clinicians the ability to judge the effectiveness of antibiotic coverage when placing an implant. Based on NNT and statistical assessments (Table 1), the present authors interpret the data to connote that there is a clinically significant benefit to prescribing an antibiotic in conjunction with implant placement with respect to reducing early implant loss in systemically healthy individuals who are not receiving bone grafts.
Regarding delineation of a specific loading dose of amoxicillin that could be used to reduce early implant loss in systemically healthy individuals who are not allergic to amoxicilin, the data is less conclusive. Nonetheless, the present authors interpret the available information described in the text to demonstrate that administration of 2 gm of amoxicillin, 1 hour before surgery, appears to provide a clinically significant reduction of early implant failures in a non-allergic, systemically healthy patient when no adjunctive bone grafting is performed. This recommendation could be altered as more revealing studies are published.
About the Authors
Gary Greenstein, DDS, MS
Clinical Professor, Department of Periodontics, College of Dental Medicine, Columbia University; Private Practice, Surgical Implantology and Periodontics, Freehold, New Jersey
Dennis Tarnow, DDS
Clinical Professor, Department of Periodontics, Director of Implant Education, College of Dental Medicine, Columbia University; Private Practice, Surgical Implantology and Periodontics, New York, New York
References
1. Stein K, Farmer J, Singhal S, et al. The use and misuse of antibiotics in dentistry: a scoping review. J Am Dent Assoc. 2018;149(10):869-884.
2. Bowen Antolín A, Pascua García MT, Nasimi A. Infections in implantology: from prophylaxis to treatment. Med Oral Patol Oral Cir Bucal. 2007; 12(4):e323-e330.
3. Surapaneni H, Yalamanchili PS, Basha MH, et al. Antibiotics in dental implants: a review of literature. J Pharm Bioallied Sci. 2016;8(suppl 1):S28-S31.
4. Suda KJ, Henschel H, Patel U, et al. Use of antibiotic prophylaxis for tooth extractions, dental implants, and periodontal surgical procedures. Open Forum Infect Dis. 2017;5(1):ofx250. doi: 10.1093/ofid/ofx250.
5. Ahmad N, Saad N. Effects of antibiotics on dental implants: a review. J Clin Med Res. 2012;4(1):1-6.
6. Braun RS, Chambrone L, Khouly I. Prophylactic antibiotic regimens in dental implant failure: a systematic review and meta-analysis. J Am Dent Assoc. 2019;150(6):e61-e91.
7. Esposito M, Grusovin MG, Worthington HV. Interventions for replacing missing teeth: antibiotics at dental implant placement to prevent complications. Cochrane Database Syst Rev. 2013;(7):CD004152.
8. Singh Gill A, Morrissey H, Rahman A. A systematic review and meta-analysis. Evaluating antibiotic prophylaxis in dental implants and extraction procedures. Medicina (Kaunas). 2018;54(6). pii: E95.
9. Ata-Ali J, Ata-Ali F, Ata-Ali F. Do antibiotics decrease implant failure and postoperative infections? A systematic review and meta-analysis. Int J Oral Maxillofac Surg. 2014;43(1):68-74.
10. Chrcanovic BR, Albrektsson T, Wennerberg A. Prophylactic antibiotic regimen and dental implant failure: a meta-analysis. J Oral Rehabil. 2014; 41(12):941-956.
11. Lund B, Hultin M, Tranaeus S, et al. Complex systematic review - perioperative antibiotics in conjunction with dental implant placement. Clin Oral Implants Res. 2015;26 suppl 11:1-14.
12. Rodríguez Sánchez F, Rodríguez Andrés C, Arteagoitia I. Which antibiotic regimen prevents implant failure or infection after dental implant surgery? A systematic review and meta-analysis. J Craniomaxillofac Surg. 2018;46(4):722-736.
13. Ranganathan P, Pramesh CS, Aggarwal R. Common pitfalls in statistical analysis: absolute risk reduction, relative risk reduction, and number needed to treat. Perspect Clin Res. 2016;7(1):51-53.
14. McQuay HJ, Moore RA. Using numerical results from systematic reviews in clinical practice. Ann Intern Med. 1997;126(9):712-720.
15. Fair RJ, Tor Y. Antibiotics and bacterial resistance in the 21st century. Perspect Medicin Chem. 2014;6:25-64.
16. World Health Organization. Essential medicines and health products: antimicrobial resistance. https://www.who.int/medicines/areas/rational_use/emp_amr/en/. Accessed December 16, 2019.
17. World Health Organization. Global action plan on antimicrobial resistance. https://www.who.int/antimicrobial-resistance/global-action-plan/en/. Accessed December 16, 2019.
18. Uman LS. Systematic reviews and meta-analyses. J Can Acad Child Adolesc Psychiatry. 2011;20(1):57-59.
19. Kramer MS. Hypothesis testing and P values. In: Clinical Epidemiology and Biostatistics. New York, NY: Springer; 1988:137-145.
20. Greenstein G. Clinical versus statistical significance as they relate to the efficacy of periodontal therapy. J Am Dent Assoc. 2003;134(5):583-591.
21. Lindgren BR, Wielinski CL, Finkelstein SM, Warwick WJ. Contrasting clinical and statistical significance within the research setting. Pediatr Pulmonol. 1993;16(6):336-340.
22. BMJ Best Practice. How to calculate risk. BMJ Publishing Group. https://bestpractice.bmj.com/info/us/toolkit/learn-ebm/how-to-calculate-risk/. Accessed December 16, 2019.
23. McQuay HJ, Moore RA. Using numerical results for systematic reviews in clinical practice. Ann Intern Med. 1997;126(9):712-720.
24. Greenstein G, Nunn ME. A method to enhance determining the clinical relevance of periodontal research data: number needed to treat (NNT). J Periodontol. 2004;75(4):620-624.
25. Chatellier G, Zapletal E, Lematire D, et al. The number needed to treat: a clinically useful nomogram in its proper context. BMJ. 1996;312(7028):426-429.
26. Arduino PG, Tirone F, Schiorlin E, Esposito M. Single preoperative dose of prophylactic amoxicillin versus a 2-day postoperative course in dental implant surgery: a two-centre randomised controlled trial. Eur J Oral Implantol. 2015;8(2):143-149.
27. Caiazzo A, Casavecchia P, Barone A, Brugnami F. A pilot study to determine the effectiveness of different amoxicillin regimens in implant surgery. J Oral Implantol. 2011;37(6):691-696.
28. Brånemark PI, Hansson BO, Adell R, et al. Osseointegrated implants in the treatment of the edentulous jaw. Experience from a 10-year period. Scand J Plast Reconstr Surg Suppl. 1977;16:1-132.
29. Siddiq A, Morkel, JA, Zafa, S. Antibiotic prophylaxis in third molar surgery: a randomized double-blind placebo-controlled clinical trial using split-mouth technique. Int J Oral Maxillofac Surg. 2010;39(2):107-114.
30. Swift JQ, Gulden WS. Antibiotic therapy-managing odontogenic infections. Dent Clin North Am. 2002;46(4):623-633.
31. European Commission - Fact Sheet. New EU action plan on antimicrobial resistance: questions and answers. June 2017. https://ec.europa.eu/commission/presscorner/detail/en/MEMO_17_1723. Accessed January 2, 2020.
32. Alanis AJ. Resistance to antibiotics: are we in the post-antibiotic era? Arch Med Res. 2005;36(6):697-705.
33. Gynther GW, Köndell PA, Moberg LE, Heimdahl A. Dental implant installation without antibiotic prophylaxis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;85(5):509-511.
34. Wright J, Paauw DS. Complications of antibiotic therapy. Med Clin North Am. 2013;97(4):667-679.
35. Daly CG. Antibiotic prophylaxis for dental procedures. Aust Prescr. 2017;40(5):184-188.
36. Sollecito TP, Abt E, Lockhart PB, et al. The use of prophylactic antibiotics prior to dental procedures in patients with prosthetic joints: evidence-based clinical practice guideline for dental practitioners-a report of the American Dental Association Council on Scientific Affairs. J Am Dent Assoc. 2015;146(1):11-16.
37. Esposito M, Thomsen P, Ericson LE, Lekholm U. Histopathologic observations on early oral implant failures. Int J Oral Maxillofac Implants. 1999;14(6):798-810.
38. Alsaadi G, Quirynen M, van Steenberghe D. The importance of implant surface characteristics in the replacement of failed implants. Int J Oral Maxillofac Implants. 2006;21(2):270-274.
39. Alsaadi G, Quiryen M, Michiles K, et al. Impact of local and systemic factors on the incidence of implant failures, up to abutment connection with modified surface oral implants. J Clin Periodontol. 2008;35(1):51-57.
40. Alsaadi G, Quirynen M, Komárek A, van Steenberghe D. Impact of local and systemic factors on the incidence of oral implant failures, up to abutment connection. J Clin Periodontol. 2007;34(7):610-617.
41. Moore A. What is an NNT? Hayward Medical Publishing. https://www.whatisseries.co.uk/what-is-an-nnt/. Updated 2009. Accessed December 16, 2019.
42. Esposito M, Cannizzaro G, Bozzoli P, et al. Efficacy of prophylactic antibiotics for dental implants: a multicentre placebo-controlled randomised clinical trial. Eur J Oral Implantol. 2008;1(1):23-31.
43. Anitua E, Aguirre JJ, Gorosabel A, et al. A multicentre placebo-controlled randomised clinical trial of antibiotic prophylaxis for placement of single dental implants. Eur J Oral Implantol. 2009;2(4):283-292.
44. Esposito M, Cannizzaro G, Bozzoli P, et al. Effectiveness of prophylactic antibiotics at placement of dental implants: a pragmatic multicentre placebo-controlled randomised clinical trial. Eur J Oral Implantol. 2010;3(2):135-143.
45. Nolan R, Kemmoona M, Polyzois I, Claffey N. The influence of prophylactic antibiotic administration on post-operative morbidity in dental implant surgery. A prospective double blind randomized controlled clinical trial. Clin Oral Implants Res. 2014;25(2):252-259.
46. Abu-Ta'a M, Quirynen M, Teughels W, van Steenberghe D. Asepsis during periodontal surgery involving oral implants and the usefulness of peri-operative antibiotics: a prospective, randomized, controlled clinical trial. J Clin Periodontol. 2008;35(1):58-63.
47. El-Kholey KE. Efficacy of two antibiotic regimens in the reduction of early dental implant failure: a pilot study. Int J Oral Maxillofac Surg. 2014;43(4):487-490.
48. Tan WC, Ong M, Han J, et al. Antibiotic Study Group. Effect of systemic antibiotics on clinical and patient-reported outcomes of implant therapy-a multicenter randomized controlled clinical trial. Clin Oral Implants Res. 2014;25(2):185-193.
49. Kashani H, Hilon J, Rasoul MH, Friberg B. Influence of a single preoperative dose of antibiotics on the early implant failure rate. A randomized clinical trial. Clin Implant Dent Relat Res. 2019;21(2):278-283.
50. Romandini M, De Tullio I, Congedi F, et al. Antibiotic prophylaxis at dental implant placement: Which is the best protocol? A systematic review and network meta-analysis. J Clin Periodontol. 2019;46(3):382-395.
51. Aravena PC, Oyarzún CP, Arias MF, et al. Single-dose bioavailability for prophylactic coverage in patients undergoing dental implant surgery. Int J Oral Maxillofac Implants. 2018;33(2):419-424.
52. Schüssl Y, Pelz K, Kempf J, Otten JE. Concentrations of amoxicillin and clindamycin in teeth following a single dose of oral medication. Clin Oral Investig. 2014;18(1):35-40.
53. Tenenbaum H, Jehl F, Gallion C, Dahan M. Amoxicillin and clavulanic acid concentrations in gingival crevicular fluid. J Clin Periodontol. 1997;24(11):804-807.
54. Eick S, Pfister W, Straube E. Antimicrobial susceptibility of anaerobic and capnophilic bacteria isolated from odontogenic abscesses and rapidly progressive periodontitis. Int J Antimicrob Agents. 1999;12(1):41-46.
55. Vincent JL, Abraham E, Moore FA, et al, eds. Textbook of Critical Care. Philadelphia, PA: Elsevier; 2011:17-48.
56. Asenjo-Lobos C, Jofré JG, Côrtes MG, Manterola C. Use of antibiotics in dental implant surgery: a decision based on evidence from systematic review. Int J Odontostomat. 2015;9(1):137-147.
57. Sharaf B, Dodson TB. Does the use of prophylactic antibiotics decrease implant failure? Oral Maxillofac Surg Clin North Am. 2011;23(4):547-550.