Implant Placement When an Impacted Tooth and Supernumerary Teeth Are Present in the Maxilla
Igor V. Kaplansky, DDS; and Gregori M. Kurtzman, DDS
ABSTRACT
The presence of impacted and/or supernumerary teeth in the maxillary anterior region can cause complications when attempting to perform restorations with implants. Extracting these structures can lead to adverse issues related to the adjacent dentition and require osseous grafting to provide a base to house the planned implant, but such an approach increases treatment time and cost. In this case report, a patient presented with an impacted permanent canine oriented on the horizontal plane with several supernumerary teeth coronal to the impacted canine. CBCT analysis revealed a very thin buccal plate over the impacted supernumerary teeth. The proposed treatment followed the principles of partial extraction therapy (PET) whereby the impacted structures were treated like bone, and implants were placed in contact with them or through them to achieve the desired osseointegration and provide long-term survival of the restored implants.
Implant placement in the maxillary anterior region can be complicated, as such factors as small volume of bone between adjacent teeth and the presence of anatomical structures like the nasal fossa and maxillary sinus create restrictions to accommodate the planned implant. This challenge increases when impacted and supernumerary teeth are present. Extracting the impacted teeth has been advocated as a way to avoid implant failure due to contact between the implant and impacted tooth.
Because of the size of the void created upon removal of the impacted structures, osseous grafting to fill the void and time to heal are needed before implants can be placed. These factors lengthen the treatment time before implant placement can be initiated. Additionally, removal of the impacted teeth may compromise bone on the adjacent teeth, especially in the apical half of the tooth where, in the maxillary anterior region, the buccal bone is normally thin. If the impacted tooth is positioned either at the apical of the adjacent tooth or more apically, it may be possible to preserve the impacted tooth and allow placement of an implant that may contact the impacted structure. This approach would follow similar principles as those utilized during partial extraction therapy, referred to as PET.
PET has been used and supported in the literature to maintain buccal bone at immediate implant placement sites where the buccal plate is thin.1,2 This technique aids in preventing implant dehiscence and in maintenance of the buccal plate over time.3 Additionally, PET allows immediate implant placement without the delays typically found when socket grafting is required following extraction to obtain sufficient thickness of the buccal plate.4 A retrospective study of 128 PET cases with up to a 4-year follow-up demonstrated a survival rate of 96.1%, which is comparable to implants placed in non-PET sites, showing that implants in contact with tooth structure can integrate and be maintained.5 Other clinical systematic reviews support this finding.6
Thus, placement of an implant in contact with an impacted tooth should yield similar clinical results. With this in mind, the case presented discusses implant placement without extraction of neighboring impacted supernumerary teeth in order to avoid potential damage to the close erupted adjacent dentition and the delays osseous grafting would place on the treatment.
Case Presentation
A 35-year-old female patient presented with a chief complaint of having a "loose baby tooth" and wanting it replaced. Nothing significant was noted in the patient's medical history, and she was not on any medication and was a nonsmoker.
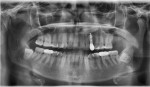
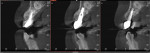
The examination noted the maxillary left deciduous canine (No. H) was present and had grade 2 mobility (Figure 1 and Figure 2). A periapical radiograph was taken and revealed a horizontally impacted maxillary left canine (No. 11) with a compound odontoma comprised of three to four small but fully formed teeth coronal to it but apical to the over-retained deciduous tooth (Figure 3). During clinical examination the supernumerary teeth could be palpated under the buccal mucosa. A cone-beam computed tomography (CBCT) scan was taken to further evaluate the situation (Figure 4). Evaluation of the CBCT sagittal view identified the impacted permanent canine oriented on the horizontal plane with several supernumerary teeth coronal to the impacted canine (Figure 5). Analysis of the CBCT's sagittal view revealed a very thin buccal plate over the impacted supernumerary teeth (Figure 6 and Figure 7).
Treatment options were discussed with the patient, who stated she was only interested in a fixed replacement. The complexity of implant placement near the impacted teeth apical to the over-retained deciduous canine was explained to her. It was further explained that removing the supernumerary teeth would destroy much of the "foundation" to accommodate implant placement and that this would require extensive grafting and a longer healing time. Because the impacted permanent canine was positioned high in the premaxilla, its position would not affect implant placement, and it was explained that this tooth would not need to be extracted. Additionally, removal of the impacted supernumerary teeth could have negative effects on the adjacent teeth compromising their stability during healing. The clinician suggested an "experimental" technique of placing the implant through impacted teeth, following similar principles of PET procedures. An impression was taken for fabrication of the provisional removable prosthesis. The patient agreed to treatment and was appointed.
Surgical Procedure
At the surgical appointment informed consent was reviewed with the patient, any questions she had were answered, and the consent form was signed. Preoperatively, the patient was administered an oral dose of 800 mg of ibuprofen and 500 mg of amoxicillin. The patient rinsed with chlorhexidine gluconate (Peridex™, 3M Oral Care, 3m.com) prior to the start of surgery. Topical anesthetic (lidocaine 10%, prilocaine 10%, and tetracaine 4%) (compounded by a pharmacy) was applied to the buccal vestibule with a cotton swab. Local anesthetic (two carpules of Articadent 4% 1:200,000 epinephrine (Dentsply Sirona, dentsplysirona.com) was administered into the buccal vestibule mesial and distal to the tooth to be extracted.
Atraumatic extraction of tooth No. H was performed with forceps. No mucoperiosteal flap was utilized, and an osteotomy was prepared to accommodate a 3.75 mm diameter implant to a depth of 13 mm, which extended into and through the impacted supernumerary teeth. An implant (Noris Tuff™, Noris Medical, norismedical.com) in size 3.75 mm x 13 mm was placed into the osteotomy, with the top of the implant's platform positioned slightly below the crestal bone (Figure 8 and Figure 9). A 2 mm healing abutment was used to allow space for the provisional prosthesis during the osseointegration phase. The prosthesis was tried in and adjusted to seat over the healing abutment such that no contact was present on the implant during the healing phase. A periapical radiograph was taken to document implant placement (Figure 10).
The patient was instructed to not disturb the implant area, including avoiding toothbrushing, for 2 weeks and to maintain a soft diet for 2 weeks, at which point she could progressively begin to eat more solid foods. She was prescribed a 7-day dose of amoxicillin 500 mg to be taken every 6 hours. She was also instructed to rinse with chlorhexidine gluconate (Peridex) twice daily for 2 weeks. A follow-up appointment was scheduled for then to check healing.
Restorative Phase
At the follow-up appointment the soft tissue demonstrated no inflammation and the patient reported having no discomfort since the last appointment. The provisional prosthesis fit was checked, and it was verified that the prosthesis was not contacting the healing abutment. The patient was scheduled in 3 months to initiate the restorative phase of treatment.
At the 3-month appointment the soft tissue around the healing abutment was non-inflamed and healthy (Figure 11 and Figure 12). The healing abutment was removed, and an Encode® abutment (ZimVie, zimvie.com) was placed and the arch scanned with an intraoral scanner (Medit i700 (wired), Medit, medit.com). The Encode abutment was then removed and the healing abutment reinserted into the implant. The case was sent electronically to a dental laboratory for fabrication of a screw-retained zirconia crown.
The patient returned 4 weeks later for restoration insertion. The healing abutment was removed. The screw-retained zirconia crown was tried in and the fit to the implant was verified radiographically. The abutment screw was tightened to 30 Ncm, per the manufacturer's recommendations. The screw channel was filled with a piece of Teflon tape, then sealed with a universal composite (Tetric® EvoCeram, Ivoclar, ivoclar.com), which was then light-cured. Occlusion was checked and adjusted as needed.
Follow-up and Long-term Results
The patient was seen at 6 months post-implant placement (1 month post-restoration) and indicated no discomfort when eating, and she was happy with the esthetic results (Figure 13 and Figure 14). At a 15-month post-implant placement recall prophy appointment, a panoramic radiograph was taken (Figure 15) and bone was noted to be in the same crestal position related to the implant platform as at initial placement. No radiolucencies were noted in or around the implant, including, specifically, where the implant was in contact with the supernumerary teeth.
The patient was seen on regular recall prophy appointments, and at the 3-year 8-month appointment post-implant placement a continuation of healthy gingival tissue with a lack of inflammation was noted around the implant (Figure 16). A periapical radiograph was taken at this appointment to check bone levels around the implant and between the implant and supernumerary teeth it was contacting (Figure 17). Additionally, a CBCT was taken to evaluate long-term the bone position in relation to the implant and the implant in relation to the supernumerary teeth. CBCT sagittal views demonstrated stability and maintenance of the bone at the crest as well as at the apical portion of the implant in relation to the supernumerary teeth (Figure 18). The axial view also confirmed maintenance of the buccal and palatal plates of the ridge in relation to the supernumerary teeth (Figure 19).
Discussion
The case presented was unique in that an impacted maxillary canine was present high in the premaxilla that would not interfere with implant placement because there was adequate ridge height apical to it and the crest. However, a compound odontoma, which consisted of multiple supernumerary teeth, was positioned in the area where the implant would need to be placed with insufficient height available to place the implant between it and the ridge's crest. As discussed, the supernumerary teeth could have been extracted, but this would have presented a high potential for negative effects to the adjacent teeth. Raising a mucoperiosteal flap and removing the supernumerary teeth would have posed a high risk of tainting the patient's nice gingival architecture and leading to tissue recession and potential loss of interdental papillae. Furthermore, grafting of the resulting defect would have been required, delaying implant placement and increasing treatment costs.
With the principles and experience reported with PET, implant contact with the supernumerary teeth was possible to avoid the potential problems outlined and accelerate the treatment timeline to completion of the final restoration. PET has been shown histologically to have integration between the root fragment and implant with no intervening soft tissue or gap reported.7,8 Because contact between the implant and supernumerary tooth is similar to a root fragment left in the site following PET, integration would be similar histologically. The long-term results of the case presented support the success of the technique illustrated.
Conclusion
Management of impacted or supernumerary teeth can pose challenges when implants are planned for the site. Extraction of those structures can create issues related to the adjacent dentition and require osseous grafting to provide a base to house the planned implant. This also increases treatment time to wait on healing of the osseous graft and cost of treatment to the patient. Following the principles associated with partial extraction therapy (PET), those impacted structures can be treated like bone, and implants can be placed in contact with them or through them to achieve the desired osseointegration and provide long-term survival of those restored implants.
ABOUT THE AUTHORS
Igor V. Kaplansky, DDS
Private Practice in Implant Dentistry, Gasport, New York; Diplomate, American Board of Oral Implantology; Fellow, American Academy of Implant Dentistry
Gregori M. Kurtzman, DDS
Former Assistant Clinical Professor, University of Maryland School of Dentistry, Baltimore, Maryland; Master, Academy of General Dentistry; Diplomate, International Congress of Oral Implantologists; Private Practice, Silver Spring, Maryland
REFERENCES
1. Ahamed MS, Mundada BP, Paul P, Reche A. Partial extraction therapy for implant placement: a newer approach in implantology practice. Cureus. 2022;14(11):e31414.
2. Karateew ED, Neiva R, Pohl S, et al. A biologic perspective on the use of partial extraction therapy in implant dentistry. Compend Contin Educ Dent. 2022;43(7):410-416.
3. Sáez-Alcaide LM, González Fernández-Tresguerres F, Cortés-Bretón Brinkmann J, et al. Socket shield technique: a systematic review of human studies. Ann Anat. 2021;238:151779.
4. Atieh MA, Shah M, Abdulkareem M, et al. The socket shield technique for immediate implant placement: a systematic review and meta-analysis. J Esthet Restor Dent. 2021;33(8):1186-1200.
5. Gluckman H, Salama M, Du Toit J. A retrospective evaluation of 128 socket-shield cases in the esthetic zone and posterior sites: partial extraction therapy with up to 4 years follow-up. Clin Implant Dent Relat Res. 2018;20(2):122-129.
6. Kotsakis GA, Nguyen TT, Siormpas K, et al; Root Membrane Group. Clinical outcomes of retention of the buccal root section combined with immediate implant placement: a systematic review of longitudinal studies. Clin Implant Dent Relat Res. 2023;25(1):23-34.
7. Shaheen RS. Partial extraction therapy: a review of the clinical and histological human studies. Int J Prevent Clin Dent Res. 2021;8(1):16-19.
8. Hürzeler MB, Zuhr O, Schupbach P, et al. The socket-shield technique: a proof-of-principle report. J Clin Periodontol. 2010;37(9):855-862.