Digital Workflow for a Definitive Implant-Supported Hybrid Prosthesis
Julian Conejo, DDS, MSc; Alejandro Sanchez-Lara, DDS; Christina Rivet; and Frank LaMar, DDS
Abstract: Implant-supported hybrid prostheses have become popular solutions when treating patients with terminal dentitions or who are completely edentulous. Since the implementation of osseointegrated dental implants to treat edentulism, multiple prosthetic designs and materials have been used for full-arch fixed hybrid prostheses. While these restorations can be highly successful, the most common restorative failures are attributed to lack of prosthetic space or a framework without passive fit, consequently leading to possible chippings, delamination, and/or fractures. This article reviews the clinical and laboratory steps for fabrication of definitive implant-supported hybrid prostheses with the implementation of bone reduction guides, implant osteotomy guides, and immediate provisionalization using digital manufacturing technologies.
Traditional protocols for the fabrication of a hybrid prosthesis require multiple time-consuming appointments, which can contribute to an arduous, sometimes unpleasant process for patients, clinicians, and dental technicians. Lack of adequate planning before the surgical phase of the treatment can compromise the availability of vertical prosthetic space, making it more difficult in the design phase to achieve esthetics, phonetics, function, and cleanability.
The implementation of digital technologies is making full-solution laboratory services more readily available and affordable for clinicians performing full-arch implant cases. Having a support team of dental designers focusing on a prosthetically driven plan can help clinicians clearly visualize any initial space limitations and determine if and when bone reduction may be needed prior to the implant placement.
Clinical Workflow
This article describes a well-defined clinical and laboratory workflow that provides a straightforward process which can allow patients to obtain a high-quality immediate provisional restoration on the day of surgery and a definitive full-arch prosthesis delivered only 6 weeks after implant placement. The clinical and laboratory sequence is presented in a step-by-step process: (1) initial records and laboratory phase 1; (2) extractions and implant surgery; (3) Express Digital (XD) scan (Hybridge, hybridgeinfo.com) and laboratory phase 2; (4) definitive prosthesis delivery.
Step 1: Initial Records
The first clinical appointment starts with digital intraoral scans of the maxillary and mandibular arches, followed by a buccal scan of the patient's bite. The buccal scan should be made with an anterior jig to re-establish the occlusal vertical dimension in a centric relation position, and not in maximal intercuspal position, to create a stable, static, and reproducible position.
A cone-beam computed tomography (CBCT) scan is recorded using an interocclusal positioning device to avoid occlusal contacts during the imaging, which facilitates the segmentation process later. Portrait photographs of the patient at a high-smile and retracted view are made using a smart phone with a smile design application (Hybridge Smile Design App). All files are uploaded to a secure cloud-based portal (The Digital Box, Hybridge).
During lab phase 1, the laboratory team designs the patient's ideal facially driven smile. After the clinician has confirmed the new tooth set-up, the prosthetic space is measured, and the amount of bone reduction, when needed, is determined. Typically in this workflow, six implants distributed between the maxillary sinuses are planned for the upper arch, and five implants to be placed between the mental foramens are planned for the lower arch. A fully guided surgery ensures that implants are placed in the optimal prosthetic-related position and best available bone. This circumvents the need for complicated bone grafts and extra surgeries.
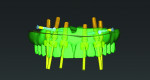
When the surgical plan is complete, the lead clinician meets with the laboratory team virtually to review and approve the guided bone reduction, implant positions, and immediate provisional to confirm that all aspects of the planning are ready for the surgery (Figure 1 and Figure 2).
Step 2: Extractions and Implant Surgery
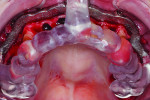
A 3D-printed metallic bone reduction guide is screwed to the jawbone (Figure 3) once its intended orientation has been determined using the occlusal indexing guide, which is used to ensure that the bone reduction guide is fixated in the correct position. The occlusal indexing guide is stabilized in the incisal and occlusal surfaces of the existing teeth. After completion of the bone reduction and extractions, an osteotomy guide is secured onto the metallic reduction guide for exacting, fully guided implant placement (Figure 4).
The clinician has the option to perform a simple polymethyl methacrylate (PMMA) conversion to allow the patient to leave the appointment with a fixed provisional and a new smile on the day of the surgery (Figure 5). As an alternative to a chairside pickup, a photogrammetry digital impression of the implants can be made and shared with the laboratory for immediate design of the fixed provisional, which can then be 3D-printed in-house. This approach is becoming more common, as a high percentage of dental clinics performing full-arch prostheses are equipped with 3D printers.
Step 3: XD Scan
At 2 to 3 weeks post-surgery, the immediately loaded provisional is unscrewed for suture removal. Scannable analogs are screwed into the provisional, and the XD scan, an extraoral scan of the provisional, is made with an intraoral scanner to transfer the implant positions to the software (Figure 6 and Figure 7). This technique reduces over-scanning and can be more time efficient when compared to intraoral scanning of scan posts in full-arch cases, especially when working with patients who present with limited aperture or when tongue and cheek retraction is difficult. To compensate for soft-tissue remodeling, an intraoral scan of the soft tissues is also made (Figure 8). This scanning sequence is more efficient than scanning the scan posts intraorally because adjacent movable structures like the tongue, lips, cheeks, and floor of the mouth are not present.
In lab phase 2, the laboratory team designs the patient's definitive prosthesis, consisting of a 3D-printed cobalt-chromium (Cr-Co) framework and milled splinted PMMA teeth. After the prothesis is thoroughly inspected, pink gingival material is applied and finished manually (Figure 9 and Figure 10). This facilitates an intimate adaptation and fusion of the white and pink PMMA surfaces so as to avoid delamination and microleakage.
Step 4: Definitive Prosthesis Delivery
The XD definitive prosthesis (Hybridge) combines an intraoral cemented interface of the titanium (Ti)-bases with the framework for absolute passivity. Cementation of the components is achieved with a self-curing resin cement (Multilink Implant, Ivoclar, ivoclar.com) to provide sufficient working time and facilitate easy excess removal. If a photogrammetry impression is available, the laboratory can fabricate a framework with a milled interface, without any cemented components.
The Cr-Co metallic framework is flexure resistant and permits a relatively long distal cantilever extension of up to two teeth, which enables improved masticatory function. This allows all the implants to be placed between the limiting anatomical structures on the maxilla and mandible. The milled PMMA teeth provide a lightweight, natural feel, and the pink acrylic gingiva material can be easily relined chairside if any phonetic challenges or food impaction areas manifest over time (Figure 11 through Figure 16).
Conclusion
The clinical workflow described is a validated treatment modality that offers clinicians the possibility of delivering a definitive prosthesis to their patients 6 weeks after implant placement. The rigidity of the framework and the intraoral cementation technique provide optimal passivity, reducing stress to the surrounding bone, which is crucial in the early osseointegration period. With the high accuracy of digital photogrammetric impressions, the same concept can be utilized without cemented components.
Acknowledgment
The authors thank the entire team at Hybridge Full Arch Laboratory for the support throughout this case.
Disclosure
Dr. Sanchez-Lara, Ms. Rivet, and Dr. LaMar (founder) are employees of Hybridge Full Arch Laboratory and/or Hybridge Implant and Smile Restoration Centers.
About the Authors
Julian Conejo, DDS, MSc
Assistant Professor, Clinical Restorative Dentistry, and Director, Chairside CAD/CAM Dentistry, Department of Preventive and Restorative Sciences, University of Pennsylvania School of Dental Medicine, Philadelphia, Pennsylvania
Alejandro Sanchez-Lara, DDS
Assistant Professor, Department of Prosthodontics, Eastman Institute for Oral Health, University of Rochester, Rochester, New York; Clinical Director, Hybridge Implant and Smile Restoration, Rochester New York
Christina Rivet
Vice President of Laboratory Innovation, Hybridge Full Arch Laboratory, Rochester, New York
Frank LaMar, DDS
Founder, Hybridge Full Arch Laboratory and Hybridge Implant and Smile Restoration Centers, Rochester, New York
BIBLIOGRAPHY
1. Conejo J, Atria PJ, Schweitzer D, Blatz MB. Digital implant planning and surgical guides: tools for clinical success. Compend Contin Educ Dent. 2021;42(7):400-401.
2. Conejo J, Yoo TH, Atria PJ, et al. In vitro comparative study between complete arch conventional implant impressions and digital implant scans with scannable pick-up impression copings. J Prosthet Dent.2024;131(3):475.e1-475.e7.
3. Conejo J, Miravete S, Jean KH, et al. Digital implant therapy for the edentulous patient. Compend Contin Educ Dent. 2022;43(10):670-673.
4. Papaspyridakos P, Bedrossian A, Kudara Y, et al. Reverse scan body: a complete digital workflow for prosthesis prototype fabrication. J Prosthodont.2023;32(5):452-457.
5. Joensahakij N, Serichetaphongse P, Chengprapakorn W. The accuracy of conventional versus digital (intraoral scanner or photogrammetry) impression techniques in full-arch implant-supported prostheses: a systematic review. Evid Based Dent. 2024. doi: 10.1038/s41432-024-01045-z.
6. Yan Y, Lin X, Yue X, Geng W. Accuracy of 2 direct digital scanning techniques - intraoral scanning and stereophotogrammetry - for complete arch implant-supported fixed prostheses: a prospective study. J Prosthet Dent. 2023;130(4):564-572.
7. Revilla-León M, Barmak AB, Lanis A, Kois JC. Influence of connected and nonconnected calibrated frameworks on the accuracy of complete arch implant scans obtained by using four intraoral scanners, a desktop scanner, and a photogrammetry system. J Prosthet Dent. 2024:4:S0022-3913(24)00048-9.