The Role of Proper Nutrition for Patients Undergoing Periodontal Surgery: A Scoping Review
Nadine M. Tassabehji, PhD, RDN, LDN; Yu-Fang Lao, MS, RD; and Irina F. Dragan, DDS, DMD, MS, eMBA
Nutrition has been recognized as a foundation for good oral health and general health, with a bidirectional relationship having been established between nutrition and oral and overall health.1 Various specific macro- and micronutrients from the intake of food serve as fuel for a person's body to grow and function.1 The oral cavity plays the unique role of gatekeeper, providing the pathway of nutrition to the body. Because of the rapid cell turnover of oral mucosa, the oral cavity also may manifest early signs of nutrient deficiencies as well as other indicators of systemic disease.2 As a result, problems in the oral cavity can profoundly affect one's appetite, desire and ability to eat, and, consequently, nutritional status and overall health.1
A healthy oral cavity encompasses more than well-functioning teeth. Firm gingival tissues with strong supporting bones, good saliva flow, and absence of tooth decay are all markers for a healthy oral cavity. According to the American Dental Association's (ADA) policies and recommendations on diet and nutrition, proper nutrition and healthy eating habits (eg, avoiding continuous intake of sugar, processed carbohydrates, and foods with low pH level) are essential to promote oral health.3 While the Academy of Nutrition and Dietetics (AND) and the ADA recommend a balanced diet for optimal general and oral health, certain nutrients and foods are often highlighted for their abilities to enhance teeth and gingival structures.4,5 Micronutrients such as calcium and phosphorus play an integral role in remineralization of enamel and can be found in food sources like milk, cheese, yogurt, poultry, eggs, tofu, and more.6 Fruits and vegetables rich in vitamin C, vitamin E, and vitamin A also introduce fiber and antioxidants into the diet to promote gingival health.7 Nevertheless, both AND and ADA agree that a balanced diet that incorporates all food groups (fruits, vegetables, whole grains, protein, dairy) is recommended to promote both oral and overall health. Unfortunately, many Americans fall short in meeting their daily requirements.8
Nutrition and Periodontal Health
Over the course of a lifetime, people are exposed to environmental factors that lead to periodontal disease, tooth decay, and tooth loss. Periodontal disease is one of the most prevalent oral diseases. According to an analysis on periodontitis using the 2009-2014 National Health and Nutrition Examination Survey, 42% of adults aged 30 years and older in the United States have some form of periodontal disease.9 The prevalence of periodontal disease increases with age as well, as severe periodontitis was most prevalent among adults aged 65 years and older.9 Besides age, common risk factors such as tobacco use and poor nutrition are also significantly correlated with periodontal diseases. Poor nutrition that lacks essential nutrients to strengthen the body's immune system is associated with worsening conditions for gums.10
Chronic disease states predispose patients to higher rates of periodontal disease. For example, more than 95% of type 2 diabetic patients have some periodontal destruction.11 Cardiovascular disease (CVD) patients are also at higher risk for periodontal and peri-implant diseases, and an increased risk of CVD is associated with periodontal disease independent of sex.12 Considering that an increasing number of patients are choosing implant-supported restorations to restore edentulous areas, the integration of nutrition guidelines may help facilitate long-term success. Also, essential nutrients can enhance implant osseointegration10 as well as long-term maintenance of the overall implant-supported prosthesis.
Moreover, many people who have periodontal diseases may require surgical interventions as treatment. These could include mucogingival corrections, regenerative procedures, dental crown lengthening, and/or resective procedures. The severity of the surgeries vary for different individuals and may lead to a wide range of postoperative surgical wounds that impact nutrient consumption.13
Complications after surgery, such as bleeding, pain, soreness, and more, could be barriers for patients to maintaining a healthy oral intake and balanced diet.14,15 With adequate nutrition being essential for wound healing, and oral pain impacting food choices and chewing and swallowing capabilities, there is a clear bidirectional relationship between nutrition and oral health (Figure 1). Impaired nutrition status can also affect postoperative recovery and delay wound healing. For patients who are elderly or medically compromised, optimizing nutrition status after periodontal surgeries becomes even more significant.16
Nutrition plays a critical role in both prevention of periodontal disease and healing after periodontal surgeries.17 Currently, numerous studies have looked at nutrition and its impact on oral health or specific nutrients and their potential benefits for promoting recovery post-surgery.17 The present authors evaluated current research available on the effects of including nutrition intervention and counseling as part of discharge instructions on postoperative recovery for patients undergoing periodontal surgical treatments.
Methods
With the support of an expert librarian, the authors conducted a search on PubMed and Embase database searching terms that included the keywords "diet therapy" OR "nutrition therapy" AND "periodontal surgery" OR "gum health" AND "postoperative period" OR "wound healing." The timeline was December 2002 to December 2022. All publications published in English in this time period were included. The publications excluded were non-human trials. Studies were excluded if nutrition was not included as a part of intervention after periodontal procedures.
The initial search yielded 76 total publications. The three authors independently screened the titles and abstracts to check inclusion criteria. Following this review a total of five citations were captured. Given the abstracts being highly relevant to the authors' subject interest, a forward and retrospective search was conducted on Web of Science, which identified two additional articles, providing a total of seven articles. The complete text of all publications fulfilling the inclusion criteria was obtained and included in the review (Figure 2).
Results
Two of the articles included in the authors' search looked at food frequency questionnaires and correlated patterns of eating specific foods and postsurgical periodontal healing.4,18 Sparrow et al found that increased intakes of different flavonoids reduced the need for scaling and root planing (SRP).18 Dodington et al found that consuming ≥1 g protein/kg body weight/day was associated with reduction in periodontal disease burden.4 Those authors did not differentiate between plant and animal sources of protein. Two articles reviewed providing commercial-based supplements to patients undergoing periodontal surgery.17,19 Typically, commercial nutrition supplements provide an array of nutrients (eg, carbohydrates, protein, fats, vitamins, and minerals). Lee et al found that after 8 weeks the intervention group that received a dietary oral supplement (increased intake of protein, vitamin A, vitamin B1, and niacin) had decreased gingival index and improved tooth mobility.19
Only one study looked at specific micronutrient supplementation. Neiva et al provided patients with vitamin B complex and found that wound healing improved for those undergoing access flap surgery. The vitamin B complex supplement included 50 mg of each of thiamine hydrogen chloride (HCl), riboflavin, niacinamide, d-calcium pantothenate, and pyridoxine HCl; 50 mcg each of d-biotin and cyanocobalamin; and 400 mcg of folate.20 Nutrients such as omega-3 fatty acids, zinc, and vitamin C are associated with anti-inflammatory properties and are positively correlated with healing and maintaining periodontal health post interventions, both surgical and nonsurgical.17
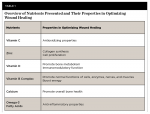
This information is important when considering a periodontal procedure that involves multiple sites. Figure 3 highlights the correction of mucogingival deformities (lack of keratinized tissue and root coverage) using an autogenous tissue from the palate. Integrating a soft diet is key for the postoperative care of this type of treatment. When a patient presents with two surgical sites, the expert advice of a dietitian that takes into consideration the patient's medical and social histories is valuable. Table 1 summarizes nutrients identified in this scoping review and their key roles in wound healing.
Discussion/Significance
Current studies have mostly focused on specific macro- and micronutrients and their potential associations with periodontal health. Moreover, many studies have examined associations between nutrition and nonsurgical periodontal interventions such as SRP, which typically do not involve prolonged healing and/or significant postoperative complications, as opposed to more invasive periodontal surgeries. Among studies that looked at more invasive periodontal procedures (eg, crown lengthening, flap surgery, grafting), none addressed general dietary guidelines or customized nutritional interventions (eg, dietary counseling, supplementation) post surgeries to examine their potential role in optimizing postsurgical healing and nutrition status. The present scoping review has revealed that there is sparse evidence regarding the influence of dietary intake as it relates to outcomes of periodontal healing after surgical procedures. Furthermore, guidelines to implement these findings in a clinical dental setting are recommended.
Periodontal disease often requires surgical interventions and yields different degrees of pain and soreness post treatment. With its essential role in aiding oral health and general health, nutrition is an integral part of postoperative care to promote recovery and healing. This study examined current findings regarding the effects of including nutrition intervention as part of discharge notes on postoperative recovery for patients undergoing periodontal surgeries. Its findings may assist dental practitioners in developing evidence-based treatment plans and discharge instructions for patients requiring periodontal surgeries in various settings, including dental schools, private practice, and hospitals. Moreover, this study may enable opportunities for care to be provided in an interdisciplinary approach in which neither periodontium health nor nutrition status is compromised.
Future research should focus on the role of specific nutrients in post-periodontal surgery and healing. Next steps include validating and implementing patient information sheets to obtain patient feedback on whether their individualized postoperative nutrition recommendations were helpful and easy to implement. Lastly, it would be beneficial to eventually be able to correlate surgical oral health outcomes with balanced and adequate nutrition of periodontal patients.
About the Authors
Nadine M. Tassabehji, PhD, RDN, LDN
Assistant Professor, Department of Comprehensive Care, Tufts University School of Dental Medicine, Boston, Massachusetts; Assistant Professor, Division of Nutrition Interventions, Communication, and Behavior Change, Friedman School of Nutrition Science and Policy, Boston, Massachusetts
Yu-Fang Lao, MS, RD
Clinical Dietitian, Martin Luther King Jr. Community Hospital, Los Angeles, California
Irina F. Dragan, DDS, DMD, MS, eMBA
Adjunct Associate Professor of Periodontology, Tufts University School of Dental Medicine, Boston, Massachusetts; Lecturer, Department of Oral Medicine, Infection, and Immunity, Harvard School of Dental Medicine, Boston, Massachusetts; Private Practice limited to Periodontology and Implant Dentistry, Boston, Massachusetts
REFERENCES
1. US Dept of Health and Human Services. Oral Health in America: A Report of the Surgeon General. Rockville, MD: US Dept of Health and Human Services, National Institute of Dental and Craniofacial Research, National Institutes of Health; 2000.
2. Tolkachjov SN, Bruce AJ. Oral manifestations of nutritional disorders. Clin Dermatol. 2017;35(5):441-452.
3. American Dental Association. Current policies: diet and nutrition. ADA website. Updated August 3, 2021. https://www.ada.org/about/governance/current-policies#dietnutrition. Accessed July 18, 2024.
4. Dodington DW, Young HE, Beaudette JR, et al. Improved healing after non-surgical periodontal therapy is associated with higher protein intake in patients who are non-smokers. Nutrients. 2021;13(11):3722.
5. Palmer CA, Boyd LD. Nutrition, and the periodontium. In: Diet and Nutrition in Oral Health. 3rd ed. Upper Saddle River, NJ: Pearson Prentice Hall; 2016:283-291.
6. Beaudette JR, Fritz PC, Sullivan PJ, et al. Patients undergoing periodontal procedures commonly use dietary supplements: a consideration in the design of intervention trials. Clin Exp Dent Res. 2021;7(1):123-128.
7. American Dental Association. Research Services and Scientific Information, ADA Library & Archives. Nutrition and oral health. ADA website. Updated August 30, 2023. https://www.ada.org/resources/research/science-and-research-institute/oral-health-topics/nutrition-and-oral-health. Accessed July 18, 2024.
8. Snetselaar LG, de Jesus JM, DeSilva DM, Stoody EE. Dietary Guidelines for Americans, 2020-2025: understanding the scientific process, guidelines, and key recommendations. Nutr Today. 2021;56(6):287-295.
9. Eke PI, Thornton-Evans GO, Wei L, et al. Periodontitis in US adults: National Health and Nutrition Examination Survey 2009-2014. J Am Dent Assoc. 2018;149(7):576-588.e6.
10. American Academy of Periodontology. Gum disease risk factors. AAP website. https://www.perio.org/for-patients/gum-disease-information/gum-disease-risk-factors/. Accessed July 18, 2024.
11. Singh M, Bains VK, Jhingran R, et al. Prevalence of periodontal disease in type 2 diabetes mellitus patients: a cross-sectional study. Contemp Clin Dent. 2019;10(2):349-357.
12. Leng Y, Hu Q, Ling Q, et al. Periodontal disease is associated with the risk of cardiovascular disease independent of sex: a meta-analysis. Front Cardiovasc Med. 2023;10:1114927.
13. A S, Tanwar E, BM D, et al. Postoperative complications after periodontal surgery. Int J Applied Dent Sci. 2018;4(4):152-156.
14. Palmer CA, Boyd LD. Oral and nutritional concerns for individuals with special medical and healthcare needs. In: Diet and Nutrition in Oral Health. 3rd ed. Upper Saddle River, NJ: Pearson Prentice Hall; 2016:390-413.
15. Watt RG, McGlone P, Kay EJ. Prevention. part 2: dietary advice in the dental surgery. Br Dent J. 2003;195(1):27-31.
16. Palmer CA, Boyd LD. Understanding nutrition as the foundation for general and oral health in the 21st century. In: Diet and Nutrition in Oral Health. 3rd ed. Upper Saddle River, NJ: Pearson Prentice Hall; 2016:2-26.
17. Lau BY, Johnston BD, Fritz PC, Ward WE. Dietary strategies to optimize wound healing after periodontal and dental implant surgery: an evidence-based review. Open Dent J. 2013;7:36-46.
18. Sparrow TV, Dodington DW, Yumol JL, et al. Higher intakes of flavonoids are associated with lower salivary il‐1β and maintenance of periodontal health 3-4 years after scaling and root planing. J Clin Periodontol. 2020;47(4):461-469.
19. Lee J, Park JC, Jung UW, et al. Improvement in periodontal healing after periodontal surgery supported by nutritional supplement drinks. J Periodontal Implant Sci. 2014;44(3):109-117.
20. Neiva RF, Al-Shammari K, Nociti FH Jr, et al. Effects of vitamin-B complex supplementation on periodontal wound healing. J Periodontol. 2005;76(7):1084-1091.