The Other Side of Endodontics: Vital Pulp Therapy on Mature Permanent Teeth
William B. Leibow, DDS, MSD; and Lindsay Springer, DMD, MPH, MAS
ABSTRACT
Vital pulp therapy (VPT) was once a treatment modality that was only considered for immature permanent teeth to allow for the continued development of the radicular system if the pulp was vital. With the advent of bioceramics and bioactive materials such as calcium silicate cements, the applications for VPT have greatly increased, giving dentists a treatment option other than nonsurgical root canal therapy (RCT) for mature teeth previously diagnosed to have an irreversible pulpitis. This approach can serve as a less invasive, simpler procedure than RCT while allowing for the preservation of natural tooth structure. It also may be a more amenable treatment alternative for patients than RCT. This article outlines and reviews the protocol for VPT with pulp exposure.
When talking with restorative dentists and patients, endodontists may often hear statements such as, "If I need a root canal, take the tooth out." Sometimes if the dentist wants to refer to the endodontist, the patient may not want to go to an endodontist and insist that the dentist either do the work necessary or take out the tooth. Patients also may consider root canals too costly, or that they do not work for various reasons. In some of these circumstances there may be another solution. Applying the principles and protocol used for successful vital pulp therapy (VPT) in immature permanent teeth to mature permanent teeth with irreversible pulpitis may be the answer to some of these predicaments.
The American Association of Endodontists (AAE) defines irreversible pulpitis as "a clinical diagnosis based on subjective and objective findings indicating that the vital inflamed pulp is incapable of healing" (p. 40).1 The AAE states symptomatic irreversible pulpitis has "additional descriptors [including] lingering thermal pain, spontaneous pain, referred pain," whereas it states asymptomatic irreversible pulpitis has "no clinical symptoms but inflammation [is] produced by caries, caries excavation [and/or] trauma" (p. 40).1 The recommended treatment for both diagnostic conditions is nonsurgical root canal therapy (RCT) assuming the tooth is restorable. This treatment recommendation may need to be revisited. According to Ricucci et al in 2019,"recent studies have reported successful outcomes when pulpotomy was performed in cariously exposed pulps of vital teeth that presented with the signs and symptoms of irreversible pulpitis and even apical periodontitis" over definitive RCT (p. 43).2
Applications for Vital Pulp Therapy
Originally, VPT was a treatment modality considered only for immature permanent teeth to allow for the continued development of the radicular system if the pulp was vital. Today, with the advent of bioceramics and bioactive materials such as calcium silicate cements, the applications for VPT have broadened.2,3 Dentists have treatment options other than nonsurgical RCT for mature teeth previously diagnosed to have an irreversible pulpitis. The AAE position statement on VPT suggests pulpitis may not have a distinct boundary and that utilizing the gradation of initial, mild, moderate, or severe pulpitis for a pulpal diagnosis might be more appropriate.4 VPT in mature permanent teeth with irreversible pulpitis should be considered as a treatment option. The presence of the pulp is necessary for dentinogenesis, nutrition, and immunocompetency of the tooth.3 Pulp preservation increases the mechanical resistance of the tooth and is crucial to its long-term survival.3 Under specific circumstances with proper diagnosis and techniques VPT may provide patients an opportunity to avoid more invasive dental treatment.
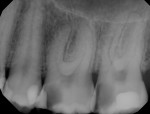
The process begins with an accurate diagnosis. Subjective patient-reported symptoms, objective clinical examination, and radiographic findings versus histological findings are used to form a clinical diagnosis for pulpal disease.5 There are numerous variables that add to the challenge of an accurate diagnosis: the patient's apprehension and past experiences, the level of pain the patient is experiencing, consumption of pain medication, as well as the clinician's ability and thoroughness. Additional consideration should be made with regard to complexity of restorative treatment when considering VPT versus nonsurgical RCT. Lin et al reported that it is better to make a diagnosis after caries excavation to determine if there is a pulpal exposure and, if so, whether the pulp is vital or necrotic.5 According to Lin et al (as cited in Mainkar and Kim, 2018), "a systematic review of the diagnosis of the dental pulp indicated that there was insufficient scientific evidence to assess the accuracy of clinical signs, symptoms or sensibility tests to determine" pulpitis.5,6 The study by Lin et al showed that there was bacterial inflammation and invasion of the pulp, but the infection approximated the caries and did not involve the entire pulp.5 Complete caries removal is necessary to resolve pulpal inflammation and increase predictability of maintaining healthy pulp tissue.2,4,5
During VPT a portion of the pulp should be removed or a complete pulpotomy performed to eliminate bacteria adjacent to the area of carious insult. The amount of pulp tissue that needs to be removed depends on bleeding.2,5 Average blood clotting time for healthy tissue is 8 to 15 minutes.5 If hemostasis is not achieved with diluted sodium hypochlorite after 5 minutes, removal of more pulp tissue is necessary. The application of diluted sodium hypochlorite is then repeated for an additional 5 to 10 minutes.5 Sodium hypochlorite is used to control hemorrhage and sanitize the dentin and pulp.1,4,5 Regardless of the method used, hemorrhage control must occur for VPT to be effective.2,5 If hemostasis cannot be achieved, nonsurgical RCT should be considered, as the pulpal inflammation likely is beyond the coronal portion of the pulp tissue.5
Vital Pulp Therapy Protocol
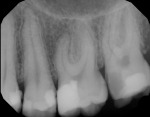
The protocol for VPT with pulp exposure is as follows (Figure 1 through Figure 13):
1. Perform a thorough diagnosis, including clinical and radiographic examinations and periodontal probing.
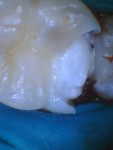
2. Place a well-sealed rubber dam.
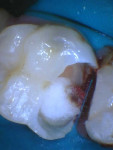
3. Excavate all caries and remove previous restorations (under magnification via scope or loupes), utilizing procedures not to further inflame the pulp (eg, use of adequate water spray, sterilized spoon excavators, and new burs). (Note: Caries detection dyes may be used. Diluted sodium hypochlorite will remove residual caries detection dyes during the sanitation process of VPT.)
4. Using a clean new diamond bur, remove 1 mm to 2 mm of pulp tissue from the area of exposure and control hemorrhage with a cotton pellet soaked in diluted sodium hypochlorite for 5 to 10 minutes.
5. If hemorrhage control is not achieved, consider the additional removal of 1 mm to 2 mm of pulp tissue or a complete pulpotomy followed by application of a cotton pellet soaked in diluted sodium hypochlorite for 5 to 10 minutes. (Note: If hemorrhaging is still not controlled, consider definitive RCT.)
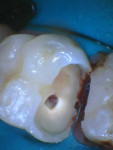
6. If hemorrhage is controlled, place self-curing calcium silicate material over the exposure against the vital pulp. (Note: Do not place a calcium silicate liner that is light-cured against the vital pulp as this will assault the pulp tissue with monomer.)
7. Place a liner that is self-curing or light-cured over the calcium silicate and restore the tooth with a definitive restoration.
8. Follow the patient for 1 to 2 months to allow time for the pulp to heal. Diagnostic testing should be used to determine the health of the pulp tissue after VPT and prior to preparing the tooth for a crown or a retainer crown for a fixed partial denture.
Conclusion
Vital pulp therapy is a less invasive, quicker, and less complicated procedure than RCT that allows for preservation of natural tooth structure and relieves pain. Additionally, because it is less complicated it should be more cost-effective for the patient, as there is less dental chairtime needed and a referral to a specialist may be unnecessary. VPT should be considered a treatment option for restorable teeth with irreversible pulpitis. Like many dental procedures, success will depend on the meticulousness of the treatment. Use of a rubber dam is imperative, and new unused burs are required for the partial pulpotomy. Proper postoperative care is essential. Some cases may need a crown depending on the remaining tooth structure and occlusal habits of the patient. Patients need to be advised that with VPT, as with any therapy involving the pulp, there is a possibility of failure, which may necessitate complete root canal treatment or possible extraction.
ACKNOWLEDGMENT
Article reprinted with permission from the Arizona Dental Association.
ABOUT THE AUTHORS
William B. Leibow DDS, MSD
Assistant Professor, Co-director of Endodontics, Arizona School of Dentistry and Oral Health, A.T. Still University, Mesa, Arizona
Lindsay Springer, DMD, MPH, MAS
Assistant Professor, Comprehensive Care Unit Director, Clinical Faculty, Arizona School of Dentistry and Oral Health, A.T. Still University, Mesa, Arizona
REFERENCES
1. American Association of Endodontists. Glossary of Endodontic Terms. Tenth ed. 2020. https://www.aae.org/specialty/clinical-resources/glossary-endodontic-terms/. Accessed May 7, 2024.
2. Ricucci D, Siqueira JF, Li Y, Tay FR. Vital pulp therapy: histopathology and histobacteriology-based guidelines to treat teeth with deep caries and pulp exposure. J Dent. 2019;86:41-52.
3. Bahcall J, Baker M. Paradigm shift in vital pulp therapy. Decisions in Dentistry. 2018;4(10):10-14.
4. AAE position statement on vital pulp therapy. J Endod. 2021;47(9):1340-1344.
5. Lin LM, Ricucci D, Saoud TM, et al. Vital pulp therapy of mature permanent teeth with irreversible pulpitis from the perspective of pulp biology. Aust Endod J. 2020;46(1):154-166.
6. Mainkar A, Kim SG. Diagnostic accuracy of 5 dental pulp tests: a systematic review and meta-analysis. J Endod. 2018;44(5):694-702.