A Modified Socket-Shield Technique: Simplifying the Root Sectioning Process
Gebin Zhu, DDS; Stuart J. Froum, DDS; Sirajuta Praisonta, DDS; Inés Fernández Guallart, DDS; Mazen Natour, DDS; Yung Cheng Paul Yu, DDS; and Sang-Choon Cho, DDS
Abstract: Socket wall resorption leading to a loss of surrounding bone following tooth extraction has been documented in the dental literature. The use of various socket-shield techniques has been suggested as a solution to this issue. In these approaches, the tooth root is sectioned in two, and the coronal two-thirds of the buccal root is preserved in the socket. This allows the periodontium along with the bundle and buccal bone to remain intact, thus preventing or minimizing bone remodeling. According to the literature, this procedure is highly technique sensitive, especially when it comes to sectioning the root. Additionally, the procedure requires significant time, and several complications may occur, such as fenestration or luxation of the remaining root, requiring its complete extraction. This case report presents a modified socket-shield technique using a trephine bur guided by a computer-designed surgical guide to simplify root sectioning, thus reducing surgical time while increasing predictability of the outcome.
Tooth extraction has been documented to result in resorption of the surrounding bone and decrease of bone mass.1 Socket-shield techniques have been proposed to mitigate this problem.2,3 These techniques involve sectioning the root into two parts, leaving the coronal two-thirds of the buccal root in the socket to preserve the periodontium, bundle bone, and buccal bone, to decrease the likelihood of bone remodeling. The socket-shield procedure is a surgical technique that aims to retain the buccal plate of an extracted tooth, which is then replaced with an implant. This approach is intended to maintain tissue volume and minimize bone resorption.
The effectiveness of this technique is heavily reliant on the technical skills of the clinician, particularly in the sectioning of the root, which is a time-consuming endeavor and may lead to complications such as fenestration or luxation of the root, necessitating its complete extraction.4
At New York University College of Dentistry (NYUCD), members of the implant department recently introduced a custom alveolar ridge technique that employs a trephine bur for splitting and grafting to enhance horizontal ridge deficiencies.5 This technique is considered less invasive and less technique sensitive than traditional methods. More recently, a modified socket-shield technique that employs a trephine bur to section the root has been used to simplify and manage the aforementioned complications of the conventional socket-shield technique.
The current case report aims to introduce a modified socket-shield technique that utilizes a trephine bur, which is guided by a computer-designed surgical guide. The purpose of this modification is to simplify the root sectioning process, thereby reducing surgical time, increasing predictability, and decreasing complications.
Materials and Methods
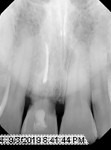
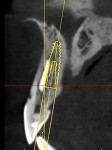
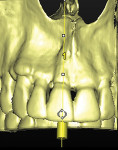
A 37-year-old male patient presented to the NYUCD Ashman Department of Periodontology and Implant Dentistry with a dental history of tooth No. 8 being avulsed in a 2014 biking accident and reimplanted with root canal treatment. In 2019 when he presented, the patient reported pain to palpation on the buccal gingiva of this tooth. The patient had no medical conditions and was not taking any medications at the time of his appointment. The clinical examination revealed a darkened tooth No. 8 (Figure 1). Radiography and a cone-beam computed tomography (CBCT) scan were performed and a 3-dimensional (3D) model was created, revealing the tooth to be ankylosed with external resorption noted along the cervical margins (Figure 2 through Figure 5). Therefore, a decision was made to extract the tooth and simultaneously place an implant.
A modified socket-shield technique would be utilized for tooth extraction and a dental implant would be placed in the socket using a 3D model simulation. All procedures were completed without any complications.
The surgical procedure was conducted using local anesthesia (1.8 mL of 2% lidocaine with 1:100,000 epinephrine). A #700 carbide fissure bur in a high-speed handpiece was used to create the initial mesial-to-distal groove through the tooth (Figure 6). This was followed by engagement of a 5-mm diameter trephine in the groove and trephining in accordance with and in the direction specified by the 3D model (Figure 7 and Figure 8). The depth of the osteotomy was predetermined based on the length of the root, and the palatal segment was atraumatically removed using periotome instruments (Figure 9 and Figure 10). The buccal segment of the tooth was preserved after tooth sectioning (Figure 11).
A second surgical guide made from the 3D model was used to create an osteotomy, and the direction and depth of the initial 2.2 mm drill was verified with a guide pin (Straumann, straumann.com) (Figure 12 and Figure 13). A slightly palatal osteotomy was then created to accommodate a 3.3 mm x 12 mm implant followed by placement of the implant (Straumann® Bone Level Tapered, Straumann). The initial stability of the implant was tested and successfully achieved (Figure 14). After the insertion of the healing abutment, a small-particle xenograft material (Bio-Oss®, Geistlich, geistlich-
pharma.com) was placed using the dual-zone technique (Figure 15).6
The patient presented 2 weeks postoperative with good healing (Figure 16). A provisional restoration was fabricated chairside using the provisional partial removable prosthesis that had been provided to the patient prior to second-stage surgery. Six weeks after implant placement, a temporary cylindrical abutment was inserted into the access hole and fixed with acrylic to create an esthetic emergence profile (Figure 17 and Figure 18).
At the 6-month follow-up appointment, the patient demonstrated stable bone levels and excellent healing of the soft tissue. Therefore, the provisional restoration was removed and the final screw-retained restoration was placed. The patient expressed satisfaction with both the esthetics and function of the restoration. He returned for regular maintenance for up to 2 years postoperatively with stable bone levels and healthy soft-tissue margins (Figure 19 and Figure 20).
Discussion
The use of the modified socket-shield technique as described resulted in a simplified procedure and successful function and esthetics of the implant at a 2-year follow-up.
The conventional socket-shield technique involves a trial-and-error approach to sectioning the root structure, which can result in less-than-ideal precision, a relatively lengthy surgical procedure, considerable invasiveness, and reduced predictability. In contrast, the modified technique presented in the current case report utilized a guided trephine to drill to a predetermined depth, which enhanced predictability and minimized the treatment time.
The trephine bur, which had a 0.3 mm thickness, facilitated highly accurate drilling, resulting in reduced mobility of the treated root and ensuring an even distance between the sectioned root and implant. This promotes uniform osseointegration of the implant surface and enables the implant to be placed palatally with excellent stability in the socket.
In addition, 3D printing technology was used to create surgical guides that provided precise guidance for the direction and positioning of the drilling process and implant placement.
Additional research with a larger dataset is required to verify the applicability of this technique.
Conclusion
Socket-shield techniques, largely regarded as technique sensitive, have been utilized to protect against socket wall resorption following tooth extraction. The modified socket-shield technique presented in this case report uses a trephine bur guided by a computer-designed surgical guide to simplify the root sectioning, thus reducing surgical time and increasing predictability. The technique may be particularly useful in the esthetic zone, where maintaining the buccal plate and tissue volume is critical for optimal outcomes. The long-term success of this technique requires careful patient selection, precise surgical performance, and regular follow-up visits to monitor the health of the implant and surrounding tissues.
Disclosure
The authors declare no conflicts of interest.
About the Authors
Gebin Zhu, DDS
Resident in Advanced Fellowship Program in Implant Dentistry, Ashman Department of Periodontology and Implant Dentistry, New York University College of Dentistry, New York, New York
Stuart J. Froum, DDS
Clinical Adjunct Professor and Director of Clinical Research, Ashman Department of Periodontology and Implant Dentistry, New York University College of Dentistry, New York, New York; Private Practice; New York, New York
Sirajuta Praisonta, DDS
Resident in Advanced Fellowship Program in Implant Dentistry, Ashman Department of Periodontology and Implant Dentistry, New York University College of Dentistry, New York, New York
Inés Fernández Guallart, DDS
Resident in Advanced Fellowship Program in Implant Dentistry, Ashman Department of Periodontology and Implant Dentistry, New York University College of Dentistry, New York, New York
Mazen Natour, DDS
Clinical Assistant Professor, Ashman Department of Periodontology and Implant Dentistry, New York University College of Dentistry, New York, New York
Yung Cheng Paul Yu, DDS
Clinical Associate Professor, Ashman Department of Periodontology and Implant Dentistry, New York University College of Dentistry, New York, New York
Sang-Choon Cho, DDS
Clinical Associate Professor and Director of Advanced Program for International Dentists in Implant Dentistry, Ashman Department of Periodontology and Implant Dentistry, New York University College of Dentistry, New York, New York
References
1. Schropp L, Wenzel A, Kostopoulos L, Karring T. Bone healing and soft tissue contour changes following single-tooth extraction: a clinical and radiographic 12-month prospective study. Int J Periodontics Restorative Dent. 2003;23(4):313-323.
2. Gluckman H, Salama M, Du Toit J. A retrospective evaluation of 128 socket-shield cases in the esthetic zone and posterior sites: partial extraction therapy with up to 4 years follow-up. Clin Implant Dent Relat Res. 2018;20(2):122-129.
3. Hürzeler MB, Zuhr O, Schupbach P, et al. The socket-shield technique: a proof-of-principle report. J Clin Periodontol. 2010;37(9):855-862.
4. Mitsias ME, Siormpas KD, Kotsakis GA, et al. The root membrane technique: human histologic evidence after five years of function. Biomed Res Int. 2017;2017:7269467.
5. Froum SJ, Kadi RO, Wangsrimongkol B, et al. The custom alveolar ridge-splitting (CARS) technique for predictable horizontal ridge augmentation in the atrophic anterior maxilla: a retrospective case series study. Int J Periodontics Restorative Dent. 2021;41(3):397-403.
6. Chu SJ, Salama MA, Salama H, et al. The dual-zone therapeutic concept of managing immediate implant placement and provisional restoration in anterior extraction sockets. Compend Contin Educ Dent. 2012;33(7):524-534.