Artificial Intelligence: A Mighty Adjunct for Caries Detection
Rena Vakay, DDS; and Gary Alex, DMD
Articifial intelligence (AI) is impacting many aspects of people's lives today. In fields such as finance, manufacturing, agriculture, insurance, education, and healthcare, AI has been commissioned to cut costs, increase efficiency, and improve accuracy. Like many innovations, the use of AI can have both positive and potentially negative consequences. As an example, if used in dentistry to detect interproximal carious lesions, AI technology does not have the ability (at least not yet) to recognize the individual uniqueness of each patient. For instance, some patients are highly caries prone and may be best served by prophylactic intervention of even small borderline lesions, while other patients are very caries resistant and may simply require the monitoring of suspected carious lesions.
Human fascination with AI is not new and existed well before the malevolent super-computer HAL from 2001: A Space Odyssey came on the scene. In 1956, the American writer Isaac Asimov wrote a science fiction short story titled, The Last Question.1 The story revolved around a first-generation self-correcting, self-adjusting computer called Multivac that was capable of learning and improving its programming. Initially, Multivac was physically huge and required a large room to hold all its components. Over decades, all the data and information humanity had to offer was processed into Multivac, which was then able to answer many questions and solve many problems confronted by humankind. Multivac enabled humans to move into space, journeying to the planets and distant stars. Over time as Multivac continued to learn, improve, and think faster, it evolved into a more compact physical form, eventually existing only as energy, moving freely through space. As billions of years passed, humankind no longer existed and the universe itself began to die as the stars burned out. Ultimately, Multivac was the only entity remaining in the dark void. Temporarily stymied on how to restore the universe back to life, Multivac ultimately determined the answer and boomed out from the void, "Let there be light!"
In this science fiction tale, Multivac represents the ultimate expression of AI, as a supreme being. Clearly, the application of the AI used in dentistry does not have this capability, but it is becoming an increasingly important and more widely utilized tool. Merriam-Webster defines AI as, "the capability of computer systems or algorithms to imitate intelligent human behavior." Copeland states, "artificial intelligence is the ability of a computer or computer-controlled robot to perform tasks that are commonly associated with intellectual processes characteristic of humans, such as the ability to reason, discover meaning, generalize, or learn from past experience."2
A Diagnostic Aid
The current use of AI in dentistry includes aiding in diagnosis of various oral diseases like dental caries, periodontal conditions, sinus problems, salivary gland diseases, temporomandibular joint disorders, and oral cancer through clinical data and diagnostic images.3 Analyzing dental radiographs for caries may be the fastest-growing area of AI use in dentistry and will be the focus of this article.
Radiographs
Historically, dental caries detection has relied on clinical evaluation by dental personnel that may include tactile, visual, magnification, photographic, and radiographic examination and interpretation. Adjuncts such as caries detecting solutions, transillumination, and laser fluorescence may also be used. The use of radiographic interpretation by AI (eg, Overjet, Logicon, Pearl, Videa Health) offers another diagnostic/screening tool. While many different types of AI exist, the radiographic interpretation of caries by computers is based on supervised learning. Supervised learning is a branch of machine learning (Figure 1)3 that involves the inputting of datasets to create computer algorithms. In terms of caries detection, one way to achieve this is for seasoned clinicians to create a dataset from many radiographs as a foundation to train a computer to make an interpretation and generate a diagnosis and course of action.4 This includes analyzing and recognizing subtle differences in opacities, translucencies, and shades of gray on dental x-rays. Simply stated, the computer learns what to look for in making its interpretation by learning patterns and being shown what is, and what is not, dental caries. Naturally, the quality, quantity, and correctness of the training data has a significant impact on the accuracy of the interpretation by the AI.
Bitewing radiographs have long been the standard for the detection and diagnosis of interproximal caries. Proper placement and angulation of the x-ray sensor to prevent overlap and/or elongation of the target teeth, along with correct exposure time, is critical. While quality bitewing radiographs are invaluable, they can also be misleading. Pre-existing radiolucent restorations, anatomic malformations, root concavities, erosive and abfraction type lesions, tooth rotations, and areas of decalcification without cavitation can all be misinterpreted by AI to be carious. This is one reason the decision to treat or not should not be based strictly on AI interpretation. AI should be considered a tool or adjunct used by the clinician to aid in final diagnosis. AI does not replace good clinical judgment and common sense. However, AI can be a powerful tool in the detection of interproximal caries. AI has the ability to quickly compare previous and future radiographs with current radiographs to determine any changes over time. Contrast enhancement can be utilized to amplify images and detail.5
Early lesion identification is a weakness of routine dental examinations but a strength of AI technology. Early lesions can often be identified and treated with preventive measures, such as sealants, chemotherapeutic agents like ICON, in-office topical fluoride and home treatments, diet counseling, and home care modification. This early intervention may save the patient time, money, and discomfort.
Caries Classification and Diagnosis
There are two classification systems for caries. The first one is based on a clinical examination of the tooth surfaces without radiographs: the International Caries Detection and Assessment System (ICDAS™).6 The second marries the clinical lesion to a radiographic evaluation: the Caries Classification System (CCS).7
The ICDAS was established in 2002 and revised in 2005. Created to standardize detection and diagnosis throughout the dental community, this system is based on the surface characteristics of a clean, dry coronal portion of the tooth.6 Codes in this system range from 0 (sound tooth structure) to 6 (extensive decay). This system is visual and identifies cavitated and non-cavitated lesions. Radiographs are not linked to the assessment.
The ICDAS utilizes a clinical examination with optimal lighting, magnification, air drying, explorer analysis, and other adjuncts to determine the true extent of the lesion and whether it is cavitated. Separation of teeth to obtain visual evaluation is sometimes indicated to better evaluate the lesion. "Frequently cavitation refers to the total loss of enamel and exposure to the underlying dentin. In any case, cavitation denotes the inability to biologically replace the loss of hard tissue, and if left untreated, the lesion is likely to progress."6
The second caries classification was released in 2008, as the American Dental Association (ADA) developed the CCS with a group of experts and the ADA Council on Scientific Affairs.7 The classification links radiographic findings with the clinical location and cavitation. It does not include risk factors of the patient. In this classification system, radiographic lesions are divided into enamel and dentin penetration, and clinical appearance is related to the radiograph. It notes that radiographs are not reliable for mild occlusal lesions. As per the ADA CCS, enamel 0 (E0) and R0 (no radiolucency) lesions have no enamel penetration. In an E1 or RA1 lesion, the lesion is in the outer half of the enamel, whereas in an E2 or RA2 lesion, the lesion extends into the inner half. D1 or RA3 lesions extend to the outer third of dentin, D2 or RB4 lesions extend to the middle third of dentin, and D3 or RC5 lesions extend into the dentin's inner third.
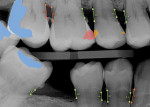
AI interprets bitewing radiographs using these caries classifications and denotes these areas with either color outlines or color fills (Figure 2). Lesions that are interpreted as E1 and E2, such as white spot lesions resulting from orthodontic treatment, need not be restored. Prophylactic treatment is warranted for E1 to E2 lesions. D1, D2, and D3 lesions require more extensive treatment.7
Implementation of Artificial Intelligence to Detect Caries
Caries diagnosis requires a combination of detection approaches. AI utilizes the comprehensive dataset of annotated bitewing radiographs.5 The caries is scored using the aforementioned caries classification systems, and a deep learning model is developed called a convolutional neural network (CNN). CNNs play an important role in efficiently aligning the radiographic caries detection and the ICDAS scores to new radiographs being interpreted.8 Using CNN increases accuracy and efficiency.8
AI can save time and effort for the clinician. Presently, AI fails to recognize the uniqueness of the patient. As stated earlier, some patients are high risk (very caries prone) and may be best served by intervention of even small borderline lesions, while low-risk patients who are caries resistant may simply require monitoring and prophylactic care of the suspected lesions, which often may never progress.
New to the AI process to most systems is the addition of photographs, patient history, and patient risk. These factors would increase the ability to predict the future risk of caries.
Some practitioners remain skeptical of AI. While a recent survey found about half of dental practitioners (51%) may be open to utilizing AI and 9% are currently using it, 14% feel it is not needed for their practices and about one-quarter of dentists (26%) are monitoring developments and considering using it.9
Ethical Considerations
The ADA is currently working on setting standards for AI and dental practices.10 Despite the value and increased utilization of AI in the dental profession, there are intrinsic weaknesses. AI may have built-in biases in decision-making and data. Additionally, artificial intelligence does not abdicate clinicians from responsible diagnosis, as it is not real intelligence and does not provide wisdom alone. An issue of liability arises when a diagnosis relies too heavily on AI alone.
Caries preventive measures are financially less rewarding to clinicians, and often there is no insurance coverage. Patients may opt out of the treatment for this reason. Since AI is still in its infancy, care needs to be taken with regard to false positives and false negatives. Some AI softwares are able to report these false positives and false negatives to the company in real-time. This is an important feature to increase the accuracy for the next generation.
With the increased development and marketing of AI, some concerns have emerged. For example, AI evaluation of x-rays is being marketed directly to patients to provide a second opinion, and this is being done without a dentist doing another clinical examination.11
About the Author
Rena Vakay, DDS
Clinical Instructor, Kois Center, Seattle, Washington; Accredited Member, American Academy of Cosmetic Dentistry; Member, American Academy of Restorative Dentistry; Private Practice, Centreville, Virginia
Gary Alex, DMD
Accredited Member, American Academy of Cosmetic Dentistry; Member, International Association for Dental Research; Private Practice, Huntington, New York
Conclusion
Artificial intelligence is still in its early development in dentistry. Use of AI should be as an adjunct and not a replacement for clinical examination and judgment. AI is not a standalone system for caries diagnosis. It is excellent for determining early lesions, which can then be treated with preventive measures. Photographs and risk assessment should be part of the process to predict future carious lesions. AI has the ability to increase efficiency and possibly improve the detection of caries, especially for less experienced dentists.
Acknowledgment
The authors thank the following people for their support and contributions to this article: Drs. John Kois, Kim Kutsch, Doug Young, and Rania Salah.
References
1. Asimov I. Multivac. The Last Question. Science Fiction Quarterly. November 1956.
2. Copeland BJ. Artificial intelligence. Encyclopedia Britannica website. December 7, 2023. https://www.britannica.com/technology/artificial-intelligence. Accessed January 9, 2024.
3. Pethani F. Promises and perils of artificial intelligence in dentistry. Aust Dent J. 2021;66(2):124-135.
4. Chen YW, Stanley K, Att W. Artificial intelligence in dentistry: current applications and future perspectives. Quintessence Int. 2020;51(3):248-257.
5. Anil S, Sudeep K, Saratchandran S, Sweety VK. Revolutionizing dental caries diagnosis through artificial intelligence. In: Chibinski AC, ed. Dental Caries - Diagnostic and Treatment Options (working title). IntechOpen website. October 19, 2023. https://www.intechopen.com/online-first/88422. Accessed January 9, 2024.
6. Gugnani N, Pandit IK, Srivastava N, et al. International Caries Detection and Assessment System (ICDAS): a new concept. Int J Clin Pediatr Dent. 2011;4(2):93-100.
7. Young DA, Nový BB, Zeller GG, et al; American Dental Association Council on Scientific Affairs. The American Dental Association Caries Classification System for clinical practice: a report of the American Dental Association Council on Scientific Affairs. J Am Dent Assoc. 2015;146(2):79-86.
8. Ding H, Wu J, Zhao W, et al. Artificial intelligence in dentistry -a review. Frontiers Dent Med. Frontiers website. February 20, 2023. Vol. 4 - 2023. https://www.frontiersin.org/articles/10.3389/fdmed.2023.1085251/full. Accessed January 9, 2024.
9. Mazda J. Trends in dentistry 2023. Inside Dentistry. 2023;19(12):12-21.
10. Versaci MB. Artificial intelligence and dentistry. ADA News website. June 7, 2023. https://adanews.ada.org/ada-news/2023/june/artificial-intelligence-and-dentistry/. Accessed January 9, 2024.
11. The TeleDentists and KELLS collaborate to introduce dental second opinions enhanced by AI evaluation. Dental Products Report website. September 13, 2023. https://www.dentalproductsreport.com/view/the-teledentists-and-kells-collaborate-to-introduce-dental-second-opinions-enhanced-by-ai-evaluation. Accessed January 9, 2024.