From Minimally Invasive Tooth Extraction to Final Chairside Fabricated Restoration: A Microscopically and Digitally Driven Full Workflow for Single-Implant Treatment
Behnam Shakibaie, DMD, MSc; Markus B. Blatz, DMD, PhD; Julian Conejo, DDS, MSc; and Huthaifa Abdulqader, DDS
Abstract: Technical advances in such fields as optical magnification (eg, loupes, microscopes), microsurgical instruments, bone and soft-tissue grafting materials, and digital dentistry have paved the way for dentists to be able to provide all the necessary specialties for a state-of-art single-tooth replacement treatment under one roof in their clinics, without having to involve a technical laboratory. This case report demonstrates a routine complete chairside digital workflow using minimally invasive and microscopic techniques in every stage of treatment, from tooth extraction and socket preservation, to implant insertion and soft-tissue management, to delivery of the final chairside digital zirconia full-anatomic supraconstruction. In addition to describing the intent of minimally invasive tooth extraction and socket preservation, this article illustrates how to perform a vestibular split rolling flap procedure and discusses its benefits. The goal of this digitally driven single-implant treatment was to achieve restoration as close as possible to the original condition.
A growing focus in periodontal-implant-prosthetic dentistry in recent years has been on minimally invasive techniques. Toward this end, preventive measures must be implemented to protect the natural anatomical structures around teeth. In state-of-the-art implantology, in an effort to circumvent subsequent augmentative measures, emphasis has been placed on reducing the inevitable resorption of the alveolar ridge that occurs before and after dental extraction. Along with this trend toward minimal invasiveness, new developments in the digital dentistry sector-in particular, chairside CAD/CAM technologies-in conjunction with newly adapted materials, have opened up conditions for the delivery of single-unit restorations with high precision and predictability in a relatively short time window.
The long-term success of implant therapy depends on various factors, including the stability of the implant bone level and the condition of the surrounding soft tissues.1,2 Additionally, the soft-tissue phenotype has been increasingly recognized as having a significant impact on the long-term outcome of the treatment.3,4 Although an autogenous connective tissue graft is considered the most effective method for augmenting soft-tissue thickness,5 in certain situations careful and precise manipulation of the existing peri-implant soft tissues can achieve the desired results. This approach can provide adequate mucosal thickness while, importantly, eliminating the need for a secondary surgical site and the associated postoperative complications.6,7 Such meticulous, precise handling of the soft tissue involves the use of techniques to enhance the thickness, width, and height of the attached mucosa.8 The most common recent method for this is the combined utilization of the vestibular split rolling flap (VSRF) and roll-in-envelope flap (RIEF) approaches, which presumably offers enhanced soft-tissue volume as well as improved overall health, esthetics, and functionality of the peri-implant tissue.9,10
This article demonstrates an established microscopically guided and digital chairside complete protocol for a single-unit implant treatment. The treatment starts with a minimally invasive tooth extraction with simultaneous socket preservation, continues with implant insertion with concurrent peri-implant soft-tissue management, and then includes a digital scan and, lastly, fabrication and delivery of the final restoration. All steps of the presented treatment protocol in the case described were executed under a surgical microscope (OPMI PROergo®, Zeiss, zeiss.com) with microsurgical (size-reduced) instruments (Figure 1).
Case Presentation
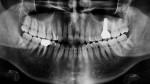
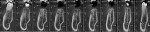
A 44-year-old healthy nonsmoking patient presented with a failing mandibular right first molar, which had been endodontically treated and restored with a fiber post and porcelain-fused-to-metal crown almost 20 years prior. After clinical and radiographic examination, secondary caries and insufficient root canal retreatment were observed (Figure 2 and Figure 3). The patient was treated in advance with a session of professional dental hygiene and treatment of multiple cavities with direct composite restorations to facilitate a clean intraoral environment before the initiation of implant-prosthetic therapy.
Minimally Invasive Extraction and Socket Preservation
Vertical root separation on tooth No. 30 was carefully performed to preserve all crucial anatomical structures of the extraction socket (Figure 4 and Figure 5). In order to minimize the inevitable ridge resorption after extraction,8,11 a socket preservation measure was implemented. The indication for such a procedure is, firstly, a fully preserved socket and, secondly, complete removal of residual inflammatory soft tissue from inside the socket, after extraction.12
The technique started with filling and packing the empty socket to the bone margin with a late-absorbing xenogenic matrix (Bio-Oss® granules, Geistlich, geistlich-pharma.com) as bone substitute material (Figure 6). Then, the bone substitute material was stabilized in place with a gelatin sponge (stypro®, Curasan, curasan.com) that also covered the entrance of the socket (Figure 7), thus supporting secondary crestal wound healing, which leads to the development of a high-quality keratinized layer of crestal mucosa.12 Finally, one horizontal crossing suture (SERALON® 6/0, Serag-Wiessner, serag-wiessner.de) was used to fix the gelatin sponge over the socket (Figure 8). The authors have found the use of this monofilament, smooth suture material to be reliable for promoting wound approximation and reducing plaque accumulation. The suture was removed after 10 days of uneventful healing (Figure 9).
The implantation should take place at least 3 months after the socket preservation technique in the case of mandibular teeth. (For maxillary teeth, the protocol typically requires an additional 2 weeks before implantation, ie, at least 14 weeks after extraction.) Attempting to use a shorter waiting period may result in an implant site that is not fully ossified and, thus, there may be a high risk for insufficient primary stability of inserted implants.11,12 In the present case, at the 3-month mark a slight resorption on the vestibular aspect with well-preserved alveolar bone was observed. When correctly executed, such techniques show significant preservation of 3-dimensional bone volume, as well as height and thickness of the keratinized gingiva, and local bone density at the time of implantation (Figure 10 and Figure 11).9
Implant Insertion With VSRF and RIEF Techniques
At 12 weeks post-extraction, a prosthetically optimal 3-dimensional (3D) implant position was analyzed using cone-beam computed tomography (CBCT) and software (Dental System™ 2018, 3Shape, 3shape.com) prior to fabrication of the 3D surgical guide, then implant surgery was initiated (Figure 11). The VSRF technique was started with the careful de-epithelialization of the vestibulocrestal part of the keratinized soft tissue in the region of the mandibular right first molar using a 1-mm-diameter round diamond bur (Figure 12). Next, angled microcrosurgical blades (Swann-Morton LTD, swann-morton.com) were used to design the outline of the flap in a rectangular shape by means of two buccolingual incisions and one mesiodistal incision (at the lingual ends of the two parallel incisions) (Figure 13). The buccolingual incisions were carefully made from the buccal line angle of the adjacent teeth, keeping a safety margin of 1 mm to 2 mm from the adjacent sulci. These incisions were performed with the intention of preserving the papillae. Also, the mesiodistal extension of the flap was made around 2 mm beyond the sagittal midline of the crest. The tunneling dissection is necessary to obtain an adequate amount of space for executing the "roll-in maneuver." The mesiodistal extension was approximately 1 mm to 2 mm beyond the crest midline to lingual. Sagitally, the flap is extended, on average, 2 mm larger than the planned diameter of the implant, with 1 mm added to both the mesial and distal sides.
The flap was then elevated using a 45-degree angled micro-elevator instrument in order to split the soft tissue while sparing the periosteum. To delicately handle the split-thickness flap, only tip-rounded microsurgical atraumatic forceps were used to perform the roll-in-envelope maneuver. By means of the same micro-elevator, the RIEF was carefully rolled in beneath the buccal soft tissue. The implant (Straumann® BLT, 4.1 mm, Straumann, straumann.com) was then placed according to the predetermined 3D plan (Figure 14). According to Shakibaie et al, the use of the roll-in-envelope technique during the VSRF approach helps ensure that the delicate microflap on the buccal aspect will remain securely in place (in the vestibular envelope) throughout the entire duration of the surgery, thus eliminating the need for a potentially risky manual holding of the microflap by an assistant or application of holding sutures that could perforate the microflap.9,10
After a thorough irrigation and cleansing of the internal part of the implant, a healing abutment was immersed in 1% chlorhexidine gel and carefully inserted into the implant fixture. Then, slight contouring of the crestolingual soft tissue was performed, and the VSRF was stabilized using two simple sutures with a 6/0 monofilament material (SERALON 6/0) (Figure 15). The sutures were carefully threaded through both layers of the rolled tissues on the buccal aspect, specifically targeting the corresponding point of the cresto-oral mucosa. This allows for the secure fixation of the RIEF in position on both the mesial and distal sides of the implant.9,10
Ten days after the surgery, healing was uneventful (Figure 16), and the sutures were removed.
Chairside-Fabricated Restoration
After 8 weeks, the patient was recalled and the peri-implant buccal musosal thickness was assessed. The reconstruction of the vestibular soft-tissue deficiency resulted in a successful outcome, characterized by an excellent natural appearance of the soft tissues (Figure 17). After confirming the presence of an optimal emergence profile upon removal of a wide-body gingiva former that had been placed, an implant scan body (Straumann BLT) was inserted and scanned via an intraoral scanner (CEREC® Primescan, Dentsply Sirona, dentsplysirona.com) (Figure 18). Then, another digital scan was recorded without the scan body to obtain the exact form of the emergence profile in order to precisely prepare a full anatomic screw-retained zirconia crown on a ti-base (Variobase®, Straumann) (Figure 19).
Right after the digital scan was taken, the full anatomic crown was designed with CEREC software and sent for milling (CEREC® Primemill, Dentsply Sirona) with a zirconia block (CEREC® Zirconia Meso Block, Dentsply Sirona). As per the patient's wishes, color A1 was selected without any individualization, and the crown was sintered in a furnace (CEREC® SpeedFire, Dentsply Sirona). The zirconia screw-retained crown was then adhesively cemented on the ti-base and polished (Figure 20). As is typical with this technique, because the designed form of the crown is slightly bigger than the original emergence profile, the try-in phase takes 30 minutes to 1 hour to form the emergence profile to the planned shape by gradually increasing pressure on the crown before final delivery (Figure 21 through Figure 24).
Conclusion
The benefits of gathering all required disciplines for a successful state-of-the-art periodontal-implant-prosthetic treatment under one roof, either in the form of a team of specialists or a multi-specialized dentist, are diverse. Implant microsurgery and microscopic and digital chairside dentistry combined with the multidisciplinary knowledge, skills, and passion of a specialist team, with the necessary time allotted, can be utilized to achieve success in highly demanding cases. Recent literature affirms that the microsurgical digital workflow is less complicated and has less risk compared with comparable conventional procedures, especially in terms of surgical segmenting of treatment. While the design, fabrication, and delivery of implant-prosthetic restorations with the latest digital chairside technologies and materials have exhibited mid-term results that are quite promising, more long-term statistics are still needed.
About the Authors
Behnam Shakibaie, DMD, MSc
Specialist in Oral Surgery, Periodontology, Implantology, and Microscopic Dentistry, Specialized Clinic in Microscopic and Digital Dentistry, Tehran, Iran
Markus B. Blatz, DMD, PhD
Professor of Restorative Dentistry, Chair, Department of Preventive and Restorative Sciences, and Assistant Dean, Digital Innovation and Professional Development, University of Pennsylvania School of Dental Medicine, Philadelphia, Pennsylvania
Julian Conejo, DDS, MSc
Assistant Professor, Clinical Restorative Dentistry, and Director, Chairside CAD/CAM Dentistry, Department of Preventive and Restorative Sciences, University of Pennsylvania School of Dental Medicine, Philadelphia, Pennsylvania
Huthaifa Abdulqader, DDS
General Dentist, Amman, Jordan
References
1. Zucchelli G, Barootchi S, Tavelli L, et al. Implant soft tissue dehiscence coverage esthetic score (IDES): a pilot within- and between-rater analysis of consistency in objective and subjective scores. Clin Oral Implants Res. 2021;32(3):349-358.
2. Stefanini M, Marzadori M, Sangiorgi M, et al. Complications and treatment errors in peri-implant soft tissue management. Periodontol 2000. 2023;92(1):263-277.
3. Barootchi S, Tavelli L, Di Gianfilippo R, et al. Soft tissue phenotype modification predicts gingival margin long-term (10-year) stability: longitudinal analysis of six randomized clinical trials. J Clin Periodontol. 2022;49(7):672-683.
4. Thoma DS, Gil A, Hämmerle CHF, Jung RE. Management and prevention of soft tissue complications in implant dentistry. Periodontol 2000. 2022;88(1):116-129.
5. Vallecillo C, Toledano-Osorio M, Vallecillo-Rivas M, et al. Collagen matrix vs. autogenous connective tissue graft for soft tissue augmentation: a systematic review and meta-analysis. Polymers (Basel). 2021;13(11):1810.
6. Tavelli L, Barootchi S, Di Gianfilippo R, et al. Patient experience of autogenous soft tissue grafting has an implication for future treatment: a 10- to 15-year cross-sectional study. J Periodontol. 2021;92(5):637-647.
7. Gobbato L, Nart J, Bressan E, et al. Patient morbidity and root coverage outcomes after the application of a subepithelial connective tissue graft in combination with a coronally advanced flap or via a tunneling technique: a randomized controlled clinical trial. Clin Oral Investig. 2016; 20(8):2191-2202.
8. Cardaropoli D, Cardaropoli G. Preservation of the postextraction alveolar ridge: a clinical and histologic study. Int J Periodontics Restorative Dent. 2008;28(5):469-477.
9. Shakibaie B, Blatz MB, Barootchi S. Clinical comparison of vestibular split rolling flap (VSRF) versus double door mucoperiosteal flap (DDMF) in implant exposure: a prospective clinical study. Int J Esthet Dent. 2023;18(1):64-79.
10. Shakibaie B, Sabri H, Blatz MB, Barootchi S. Comparison of the minimally-invasive roll-in envelope flap technique to the holding suture technique in implant surgery: a prospective case series. J Esthet Restor Dent. 2023;35(4):625-631.
11. Shakibaie B. Uses of the operating microscope in minimally invasive implantology. Quintessenz. 2010;61:293-308.
12. Shakibaie B. Socket and ridge preservation. Dental Magazine. 2009;2 (27):24-33.