An Analog Intermezzo in a Digital Workflow
Lambert J. Stumpel, DDS
Abstract: Digital dental technology has revolutionized the workflows in the dental laboratory and clinical environment. Although the novelty of digital dentistry can be alluring, clinicians should bear in mind that the overall outcome is what matters most rather than the path taken to achieve that outcome. Combining analog and digital pathways can serve to amplify each one and thus enhance the result. This article presents two case examples where an analog excursion in an otherwise digital workflow saved time and reduced cost compared to a dogmatic digital approach. In one case, an alternative workflow is presented to produce implant fixed complete dentures, and in the other case composite was used to generate the pink esthetic component for a complete denture, which could be fixed or removable.
Digital technology is increasingly becoming an integral part of the dental profession and is having a significant impact on prosthodontics. With all of the excitement and enthusiasm about digital approaches, clinicians must remember that digital prosthodontic workflows, products, and techniques are just tools to assist "analog" (ie, actual) dentists treat "analog" patients with "analog" prostheses. The objective of digital dentistry is to achieve the desired outcome faster, more economically, and better. The method by which this is obtained is subservient to this objective. Therefore, the use of the most appropriate pathway is imperative, be it digital, analog, or a combination of both.
This article describes two cases where minor analog diversions from an otherwise digital workflow proved to be beneficial.
Case 1
The prosthetic design for the first implant-supported fixed dentures in history consisted of a gold metal framework, which supported pink acrylic and conventional denture teeth.1,2 Although in dentistry today cast gold has mostly been replaced by alternatively fabricated and constituted substructures, the basic concept remains unaltered. High success rates have been reported for this nearly half-a-century-old model.3-9
Of course, prosthetic complications are to be expected, such as fracture of the acrylic teeth, fracture of the pink acrylic material, discoloration, and unstable occlusal contacts due to wear.10-13 Acrylic resin veneer fractures can be exacerbated by improper design of the substructure.14,15
To reduce the wear of the denture teeth the use of amalgam or gold alloy reinforcements of existing denture teeth has been proposed.16 Another option with excellent reported results is the fabrication of a metal substructure with individually formed aluminum oxide or zirconium oxide crowns.17-19 Other approaches have utilized zirconia even further by fabricating the complete prosthesis with zirconia, sometimes in conjunction with the esthetic layering of feldspathic porcelain.18-25 Often, however, catastrophic fractures of the prostheses have been reported,26 leading to the development of the concept of zirconia shells bonded to supporting metal substructures.27 Recently a novel technique was described where a conventional digital removable denture workflow was adapted to fabricate an implant-supported fixed complete denture comprised of a metal substructure, pink composite, and multilayered zirconia.28
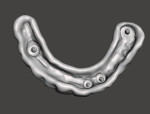
Using this technique, a metal substructure was fabricated and placed onto the cast. The cast was scanned with an intraoral scanner (Trios Move, 3Shape, 3shape.com) (a desktop scanner may also be used), and this file was entered into a removable denture software program (Dental Desktop, 3Shape). The bar was blocked out with virtual wax, excluding four areas to allow precise seating of the yet-to-be-fabricated pink denture base (Figure 1). The bar was now assumed to be part of the edentulous ridge, and a conventional prosthesis was designed in the digital denture software (Figure 2).
Because the workflow is designed for removable prostheses some alterations are required to adapt the outcome for an implant fixed prosthesis. It is not possible, for example, to use screw-access holes in the removable denture workflow but they usually are required in the fixed solution. The software generated two distinct stereolithography (STL) files: one for the denture base and one for the teeth section (Figure 3 and Figure 4). The teeth section would be milled out of multilayered zirconia (Katana™ Zirconia STML, Kuraray, kuraraydental.com), then sintered and glazed. The denture base would be printed with denture resin (Denture 3D+, NextDent, nextdent.com).
Since the denture base was tightly adapted to the four areas on the metal bar, this bar could now be precisely bonded into the intaglio side of the denture base with a universal luting resin (Panavia™ SA, Kuraray) (Figure 5). The screw-retained pink base was now able to accept the "white" teeth section. This zirconia arch was bonded with a 10-methacryloyloxydecyl dihydrogen phosphate (MDP)-containing luting composite (Panavia SA), which ensured a reliable bond between the substrates.29,30 Here is when an expedient analog segue was interjected in the otherwise digital workflow.
The teeth section was tried intraorally with burnout resin (Cast, NextDent) and try-in resin (Try-In, NextDent) (Figure 6 through Figure 8). Multiple issues were noted. After approving the original set-up, the patient requested shorter central incisors. Also, the occlusion was premature and screw-access holes were needed to access the retaining screws. Instead of returning to the digital workflow and making the required adjustments digitally, the actual printed teeth section was mechanically adjusted. The adjusted arch was then scanned with an intraoral scanner (Trios Move), and an STL file was generated (Figure 9). This STL file was used to fabricate the zirconia teeth section (Figure 10), which was then bonded per the described protocol (Figure 11 and Figure 12).
Returning to the digital workflow would have been possible once the need for modifications to the white teeth section was established, and those modifications could have been made digitally; however, this would have required considerable time and effort. Simply adjusting the computer-assisted manufacturing (CAM) output, confirming its correctness, and then rescanning the adjusted part of the restoration was more expedient in this case.
Case 2
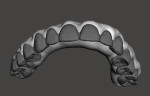
The digital denture software used in the first case can produce the distinct files used to create a prosthesis with the appearance of a conventional denture with pink gingiva and white teeth. The differentiation is driven partially by esthetics, as teeth, of course, are a different color than soft tissue. The software is also able to create a single file, a monoblock that is a combination of the teeth section and the denture base. The CAM output will thus consist of the same material for the whole prosthesis. Be it printed or milled, the prosthesis will have white teeth but also a white denture base and, most noticeably, white papillae. If the output is zirconia, pink-stained ceramics can be employed to cover up the visible areas that should be pink. If the output is milled polymethyl methacrylate (PMMA) or printed composite, the pink esthetic component is created using tissue-colored composites. Highly skilled dental technicians then cut back the gingiva and sculpt the tissue simulation around the teeth with various shades of pink composite. As an example, Figure 13 shows milled 10-layer PMMA (AnaxCAD PMMA, Anaxdent, anaxdentusa.com) with hand cut-back of the gingival area, and Figure 14 depicts the application of tissue-colored composite. This is clearly a laborious and thus expensive endeavor.
This case describes a much less artistic analog technique than described above but one that would likely be acceptable in many cases. It combines the software-generated gingival contour design with controlled manual application of pink-colored composite. In short, the gingival contour is generated in the computer-assisted design (CAD) software. A full-contour prosthesis is printed and a vacuformed shell is manufactured to capture the contour. The CAM file is adjusted to evenly reduce a small area that will need to be pink in the final prosthesis. The prosthesis is generated in the desired material, and the gingival well is filled with pink-colored composite that is contoured with the full-contour vacuformed shell.
The monoblock STL file of the prosthesis was created by means of the digital denture software (Dental Desktop) (Figure 15). This file was opened in an open-source STL manipulation program (Meshmixer, Autodesk, meshmixer.com). The first step was to make the file "solid"; this increases the mesh density so that painting the selection in the next step will be more precise, although doing this increases the file size considerably. The software sequence was: Edit, Make solid, Solid type Accurate, Solid accuracy 512, Mesh density 512, Update, Accept. Next, choose Select (keyboard S), and paint the desired area with the brush. The brush size can be adjusted in the options box or with the "[" and "]" keyboard keys. Deselection can be done by simultaneously holding the Shift key.
Once the desired area is selected, go to Edit, Extrude (keyboard D), and select an offset of -0.7 mm-1.0 mm, Accept. A uniform reduction of the selected area will now have been created (Figure 16). Pressing "B" on the keyboard will smooth the boundaries of the selected area. Further smoothing of these borders can be accomplished with the RobustSmooth brush under "Brushes" in the sculpt menu. Save this STL file. An alternative Meshmixer workflow after making the selection of the to-be-reduced area is: Modify, Optimize boundary (keyboard O), Smooth boundary (keyboard B), Accept, Edit, Offset, Distance -0.7 mm, Accept, Export file.
The file that was just created will be used to generate the CAM output in the selected milled or printed material. The output will have a uniform recessed area following the external contours as designed in the digital denture software. The clinician then prints the original file with the computer-generated soft-tissue contours and generates the CAM output denture. A flexible vacuformed shell (Essix 1.5mm MG/Model Duplication Vacuum Square, Dentsply Sirona, dentsplysirona.com) was created that covered all the external surface of the denture. A stiff polyvinyl siloxane (PVS) putty (Exaflex®, GC America, gcamerica.com) was used to create an index on the buccal aspect (Figure 17). This index will allow the application of even pressure onto the flexible vacuformed shell later.
The CAM output of the modified file was generated, creating the prosthesis with an evenly reduced area. A bonding agent was placed on the reduced area, and for composite a composite bonder was used. If a PMMA is used it is especially important to use a dedicated PMMA/composite bonder (Bond LC, Anaxdent).
Next, the desired color of pink composite (Anaxgum Pink Composite, Anaxdent) was selected and 10 mm to 15 mm of it was extruded onto a pad, rolled into a string about the length of the reduced area, and applied into the well of the CAM prosthesis. Finger pressure was used to fill the well, and instruments were then used to adapt the composite evenly (Figure 18). The vacuformed shell was then placed, and the PVS index used to apply even pressure. A small amount of composite should extrude beyond the margin of the shell; this composite is subsequently removed with an instrument (Figure 19). As needed, a small amount of composite may be added to deficient areas to allow complete generation of the contours.
Polymerization was then initiated with a handheld light polymerization unit; alternatively, the restoration can be immediately placed into a post-polymerization lightbox. The vacuformed shell can be removed and final polymerization completed. Limited finishing can be done with rotating instruments. A small amount of red and white stains (Anaxgum Paint, Anaxdent) can be applied as needed to improve the esthetic outcome. Finally, a glaze (Dreve Nanovarnish, Anaxdent) was applied, and the prosthesis polished (Pasta Grigia I, Anaxdent).
This simple workflow facilitates the generation of the visible pink esthetic component for a prosthesis that otherwise is fabricated in a monolithic material. It utilizes the morphology as generated by the digital denture software (Figure 20).
Conclusion
Digitization has rapidly changed and will continue to change dentistry as a whole. The most profound changes currently are occurring in the fabrication of indirect restorations, for which dental laboratories are mostly responsible. Clinical applications are quickly catching up in adopting digital workflows. Clinicians must realize, however, that digital dentistry should not be a goal in and of itself, but a pathway toward improved care. The purposeful combination of analog and digital paths may be a possible option to enhance outcomes.
About the Author
Lambert J. Stumpel, DDS
Private Practice, San Francisco, California
References
1. Adell R, Lekholm U, Rockler B, Brånemark PI. A 15-year study of osseointegrated implants in the treatment of the edentulous jaw. Int J Oral Surg. 1981;10(6):387-416.
2. Zarb GA, Schmitt A. The longitudinal clinical effectiveness of osseointegrated dental implants: the Toronto study. Part III: problems and complications encountered. J Prosthet Dent. 1990;64(2):185-194.
3. Balshi TJ, Wolfinger GJ, Balshi SF, Bidra AS. A 30-year follow-up of a patient with mandibular complete-arch fixed implant-supported prosthesis on 4 implants: a clinical report. J Prosthodont. 2019;28(2):97-102.
4. Jemt T, Johansson J. Implant treatment in the edentulous maxillae: a 15-year follow-up study on 76 consecutive patients provided with fixed prostheses. Clin Implant Dent Relat Res. 2006;8(2):61-69.
5. Lambert FE, Weber HP, Susarla SM, et al. Descriptive analysis of implant and prosthodontic survival rates with fixed implant-supported rehabilitations in the edentulous maxilla. J Periodontol. 2009;80(8):1220-1230.
6. Att W, Bernhart J, Strub JR. Fixed rehabilitation of the edentulous maxilla: possibilities and clinical outcome. J Oral Maxillofac Surg. 2009;67
(11 suppl):60-73.
7. Brånemark PI, Svensson B, van Steenberghe D. Ten-year survival rates of fixed prostheses on four or six implants ad modum Brånemark in full edentulism. Clin Oral Implants Res. 1995;6(4):227-231.
8. Balshi TJ, Wolfinger GJ, Slauch RW, Balshi SF. A retrospective analysis of 800 Brånemark System implants following the All-on-Four™ protocol. J Prosthodont. 2014;23(2):83-88.
9. Maló P, Rangert B, Nobre M. "All-on-Four" immediate-function concept with Brånemark System implants for completely edentulous mandibles: a retrospective clinical study. Clin Implant Dent Relat Res. 2003;5(suppl 1):2-9.
10. Gallucci GO, Avrampou M, Taylor JC, et al. Maxillary implant-supported fixed prosthesis: a survey of reviews and key variables for treatment planning. Int J Oral Maxillofac Implants. 2016;31 suppl:s192-s197.
11. Bozini T, Petridis H, Garefis K, Garefis P. A meta-analysis of prosthodontic complication rates of implant-supported fixed dental prostheses in edentulous patients after an observation period of at least 5 years. Int J Oral Maxillofac Implants. 2011;26(2):304-318.
12. Lekholm U, Jemt T. Complications and results [article in Spanish]. Arch Odonto Estomatol. 1988;4(8):416-424.
13. Jemt T. Failures and complications in 391 consecutively inserted fixed prostheses supported by Brånemark implants in edentulous jaws: a study of treatment from the time of prosthesis placement to the first annual checkup. Int J Oral Maxillofac Implants. 1991;6(3):270-276.
14. Papaspyridakos P, Chen CJ, Chuang SK, et al. A systematic review of biologic and technical complications with fixed implant rehabilitations for edentulous patients. Int J Oral Maxillofac Implants. 2012;27(1):102-110.
15. Coltro M, Ozkomur A, Villarinho E, et al. Risk factor model of mechanical complications in implant-supported fixed complete dentures: a prospective cohort study. Clin Oral Implants Res. 2018;29(9):915-921.
16. Purcell BA, McGlumphy EA, Holloway JA, Beck FM. Prosthetic complications in mandibular metal-resin implant-fixed complete dental prostheses: a 5- to 9-year analysis. Int J Oral Maxillofac Implants. 2008;23(5):847-857.
17. Maló P, de Araújo Nobre M, Borges J, Almeida R. Retrievable metal ceramic implant-supported fixed prostheses with milled titanium frameworks and all-ceramic crowns: retrospective clinical study with up to 10 years of follow-up. J Prosthodont. 2012;21(4):256-264.
18. Maló P, de Sousa ST, De Araújo Nobre M, et al. Individual lithium disilicate crowns in a full-arch, implant-supported rehabilitation: a clinical report. J Prosthodont. 2014;23(6):495-500.
19. Lin WS, Metz MJ, Pollini A, et al. Digital data acquisition for a CAD/CAM-fabricated titanium framework and zirconium oxide restorations for an implant-supported fixed complete dental prosthesis. J Prosthet Dent. 2014;112(6):1324-1329.
20. Larsson C, Vult von Steyern P. Five-year follow-up of implant-supported Y-TZP and ZTA fixed dental prostheses. A randomized, prospective clinical trial comparing two different material systems. Int J Prosthodont. 2010;23(6):555-561.
21. Pozzi A, Holst S, Fabbri G, Tallarico M. Clinical reliability of CAD/CAM cross-arch zirconia bridges on immediately loaded implants placed with computer-assisted/template-guided surgery: a retrospective study with a follow-up between 3 and 5 years. Clin Implant Dent Relat Res. 2015;17(suppl 1):e86-e96.
22. Le M, Papia E, Larsson C. The clinical success of tooth- and implant-supported zirconia-based fixed dental prostheses. A systematic review. J Oral Rehabil. 2015;42(6):467-480.
23. Larsson C, Vult Von Steyern P. Implant-supported full-arch zirconia-based mandibular fixed dental prostheses. Eight-year results from a clinical pilot study. Acta Odontol Scand. 2013;71(5):1118-1122.
24. Marchack BW, Sato S, Marchack CB, White SN. Complete and partial contour zirconia designs for crowns and fixed dental prostheses: a clinical report. J Prosthet Dent. 2011;106(3):145-152.
25. Altarawneh S, Limmer B, Reside GJ, Cooper L. Dual jaw treatment of edentulism using implant-supported monolithic zirconia fixed prostheses. J Esthet Restor Dent. 2015;27(2):63-70.
26. Chang JS, Ji W, Choi CH, Kim S. Catastrophic failure of a monolithic zirconia prosthesis. J Prosthet Dent. 2015;113(2):86-90.
27. Stumpel LJ, Haechler W. The metal-zirconia implant fixed hybrid full-arch prosthesis: an alternative technique for fabrication. Compend Contin Educ Dent. 2018;39(3):176-181.
28. Stumpel LJ, Scherer MD. Workflow for a metal-resin-zirconia fixed complete denture: a dental technique. J Prosthet Dent. 2020;S0022-3913(20)30103-7. doi: 10.1016/j.prosdent.2020.01.033.
29. Kern M, Passia N, Sasse M, Yazigi C. Ten-year outcome of zirconia ceramic cantilever resin-bonded fixed dental prostheses and the influence of the reasons for missing incisors. J Dent. 2017;65:51-55.
30. Kern M, Sasse M. Ten-year survival of anterior all-ceramic resin-bonded fixed dental prostheses. J Adhes Dent. 2011;13(5):407-410.