A Novel Surgical Aid to Achieve Optimal Positioning of Adjacent Implants in Fully Edentulous Mandibular Cases
Shalin Vinayak, DMD, MFD; Stuart J. Froum, DDS; Kuanyou Liu, DDS; Anna Corinna Lim, DDS; and Michael Liang, DDS
Abstract: The 3-dimensional implant position is critical in achieving a successful surgical and prosthetic outcome for an implant-supported restoration. In an edentulous mandibular arch, the lack of neighboring reference points and the nature of the resorptive process make ideal surgical implant placement difficult to achieve. As the edentulous mandibular ridge resorbs lingually and apically, the ideal prosthetic tooth positions often may be located facial to the ridge crest. Achieving proper implant position requires use of a guide that takes into consideration the location of the existing ridge in addition to ideal tooth position. This article describes the use of an adaptable, metal, linked implant position guide that utilizes interimplant spacing of 5 mm, 7 mm, or 9 mm between adjacent tooth positions throughout the arch to aid in keeping adjacent implants parallel and symmetrical to the contralateral side while also respecting the ideal natural tooth dimensions and occlusion. The use of the guide is demonstrated in three cases of mandibular edentulism.
A complete mandibular denture seldom provides total satisfaction to the patient, with a common complaint being lack of stability or retention.1 Dental implants are an effective option for improving function, as they provide support for an overdenture or fixed prosthesis. However, a thorough understanding of both the biology and the use of a restoratively driven approach is necessary to achieve favorable outcomes.2-4
The 3-dimensional (3D) position of the implant is an important factor in attaining a long-term successful result.5-7 According to the literature, to avoid crestal bone loss during the establishment of the implant biologic width, a distance of at least 1.5 mm must be maintained from the implant to adjacent teeth,8 2 mm from the implant to facial and lingual plates,9 and 3 mm between adjacent implants.10,11 Correct biomechanical positioning helps to ensure a uniform distribution of occlusal forces between the implants and minimize non-axial forces placed on the implant. From an esthetic perspective, correct implant position allows for an ideal emergence profile and crown contours similar to that of a natural tooth.11-13
In sites of a single tooth replacement, 3D implant position is determined based on the neighboring teeth or implants.14,15 Fully edentulous mandibular arches present more of a challenge due to the lack of neighboring reference points and the nature of the resorptive process. The edentulous mandibular ridge resorbs lingually and apically, resulting in ideal prosthetic tooth replacements being placed facial to the ridge crest.16 However, implants are usually placed in the edentulous ridge where the bone volume is greatest. Therefore, other factors besides tooth position must be considered during treatment planning. Attention must be given to planning parallel adjacent implants at sufficient distance from each other and from the buccal and lingual cortical plates, and to maintaining symmetry in the arch while adhering to the principles of 3D implant position.17
Various types of surgical guides have been used to achieve accurate implant position and minimize errors that can arise when freehanded, unguided surgery is performed.18 All of these, however, have limitations. A duplicated denture or ideal tooth set-up-based guide may be difficult to seat once a flap has been raised, thus making the task of accurately locating the midline difficult. Moreover, sufficient bone is seldom available at the ideal tooth location in long-standing edentulous mandibles.16 In these situations, the duplicated denture guide is of limited value and its use may result in asymmetry and lack of parallelism between implants.19 Cone-beam computed tomography (CBCT)-based custom fabricated guides are more accurate.20 However, they take time to fabricate, increase cost, and require a greater amount of intraoral vertical room; moreover, studies have shown they can limit the amount of irrigant to the osteotomy when used with a flapless approach.21 Furthermore, for completely edentulous cases, it becomes more complex for digital workflows to overcome the limitations of intraoral scanning in arches without teeth to serve as reproducible landmarks.22
This article demonstrates the use of a flexible linked implant positioning (FLIP) guide to overcome the limitations of freehanded and conventional guided surgery, allowing for parallel implant positioning for a two-implant overdenture and partial- or full-arch implant-supported restoration.
Materials and Methods
The FLIP guide (produced and patented [US8, 491, 301, B2] by EBI Implant North America, ebiimplantusa.com) expands on the work of McArthur and Wheeler, who stated the ideal anatomical tooth dimensions.23 From these dimensions, the distance between the centers of adjacent teeth, representing the location of adjacent osteotomies, was determined. These dimensions on average were 5 mm, 7 mm, or 9 mm between adjacent tooth positions throughout the arch, with 5 mm being the average distance between mandibular incisors, 9 mm between molars, and 7 mm between the remaining teeth (Figure 1).
In the present case series, the FLIP guide was used as a surgical aid to allow adjacent osteotomies to be created parallel to each other at distances of 5 mm, 7 mm, or 9 mm. Three cases are shown that demonstrate the guide's use for placement of implants into edentulous mandibles for a one- or two-stage mandibular overdenture and a full-arch fixed prosthesis.
The FLIP guide is comprised of individual metal segments of the three proposed dimensions (Figure 2). Each segment has a 2-mm diameter drill-guiding sleeve at one end and a linking apparatus at the other, allowing the guide to be attached to an adjacent segment. Segments can be linked together at either side of the midline based on the location of the most distal implant, and the guide may be bent to conform to the shape of the dental arch (Figure 3). This enables placement of between two to nine implants in positions that correspond to the ideal tooth position (Figure 4). The resulting symmetry on either side of the midline, optimal interimplant spacing, and parallelism allows for uniform distribution of force between implants and simplifies the prosthetic procedures when restoring them.24
Surgical Procedure
Case 1
An 83-year-old edentulous woman presented with a chief complaint of an uncomfortable lower denture that moved when she talked or ate, and she desired a solution that fit better to allow her to chew better. On examination of the patient a very shallow vestibule was found that was limiting the denture flanges from being properly extended. A plan, therefore, was proposed to place two implants in the mandibular canine positions with Locator® attachments (Zest Dental Solutions, zestdent.com) to aid in stability, support, and retention of the prosthesis.
A CBCT scan was taken with a radiographic template made from a duplicate of the patient's denture (Figure 5). The CBCT, along with treatment-planning software (Simplant 17 Pro, Dentsply Sirona, dentsplysirona.com), was used to confirm that a sufficient volume of bone was available at the desired implant positions and to identify vital anatomic landmarks (Figure 6). The FLIP guide was then assembled chairside in preparation for the surgery. When planning for a two-implant overdenture, as in this case, fewer segments of the guide are required.
The guide was placed on the ridge and secured in position by placing the initial drill through the midline (Figure 7). The flat topography of the ridge allowed stable seating of the guide, which was secured in position through the midline osteotomy (Figure 8). Because no ridge contouring was needed, a flapless surgical approach could be used. Use of the guide helped ensure parallelism and equidistance from the midline (Figure 9 and Figure 10), which has been shown to enable use of more retentive overdenture attachments with less wear.24
Case 2
In case 2 the patient presented with a "knife-edge" morphology of the mandibular ridge (Figure 11). When alveoplasty is required to increase crestal width or to allow for stable seating of the guide, as was necessary in this case, a full-thickness flap is elevated to expose the ridge (Figure 12). Bony irregularities in the ridge were reduced using a bur (Ridge Contouring Bur, EBI Implant North America) with a surgical handpiece at 2000 rpm under copious saline irrigation to attain a flat surface upon which the guide, and subsequently the denture, will sit (Figure 13).
Parallelism of adjacent osteotomies and equidistant spacing from the midline were achieved, as demonstrated by the position of the respective 2-mm twist drills placed through the guide (Figure 14). The minimally obtrusive guide enabled adequate visualization and access for irrigant to the osteotomy.
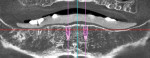
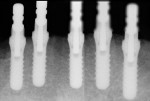
Adjacent implants were then placed parallel to each other and equidistant from the midline, in an ideal position to receive overdenture attachments. Cover screws were placed, and the flap re-placed (Figure 15). A radiograph taken immediately after placement verified the parallelism of the two implants placed with the aid of the FLIP guide (Figure 16).
Case 3
Case 3 represents a full-arch implant restoration. Links of all three sizes-5 mm, 7 mm, and 9 mm-were connected together at their respective positions corresponding to the ideal position of the natural teeth to allow placement of up to nine implants throughout the arch. In this case six implants were placed (Figure 17). The FLIP guide was seated and secured to the crest of the ridge using a surgical bur through the midline, which is left in place while the osteotomies are created. The initial osteotomies were made through the guiding holes at the corresponding tooth positions and at suitable interimplant distances. The guide was then removed, and osteotomies were completed to final depth and diameter.
The implants were placed parallel to each other and radiographs were taken to verify final position (Figure 18). The parallelism and appropriate interimplant spacing allowed for ease of prosthetic connection of a screw-retained provisional restoration (Figure 19).
Discussion
Long-standing mandibular edentulism presents a challenging situation to clinicians attempting to restore form and function. Conventional removable dentures seldom provide complete satisfaction for the patient, with the mandibular denture being the source of most complaints. A two-implant-supported restoration, therefore, has been proposed as the minimum standard of care when restoring edentulous mandibular ridges.24,25 Furthermore, implants can be used to provide a full-arch fixed prosthesis that offers improved stability and allows greater ability to chew.25,26
The 3D implant position is critical in achieving a successful result, as it has great influence on the outcome of treatment.14,15 Parallel implant placement, whether for a two-implant overdenture or a multi-implant restoration, is important because it avoids an imbalance of occlusal forces within the restoration that can lead to loosening or breakage of abutment screws in a fixed restoration or excessive wear of components in a removable restoration. Furthermore, parallel implants allow for ease of prosthetic fabrication and enable a simple path of insertion with highly retentive attachments to retain a removable prosthesis. For a full-arch restoration, this parallelism between implants provides the ability to use a screw-retained provisional or final restoration. Symmetry to the contralateral side is achieved by placing implants equidistant from the midline, allowing for uniform distribution of forces throughout the arch. With the use of the FLIP guide, implants can be placed at the ideal position to preserve the interimplant bone.
Conventional surgical guides are either based on duplication of a dental prosthesis or vacuum-formed over a wax-up. Although they are convenient to use as they can be fabricated relatively quickly and inexpensively, their clinical benefit may be limited because the osteotomy is created using a freehanded approach, which is dependent on the clinician's experience and skill to achieve parallelism and correct positioning. The clinical benefit of conventional surgical guides is further limited in cases of ridge atrophy, when the ideal prosthetic tooth positions are not located directly above the ridge crest.
The guide used in the presented cases offers the convenience of being a non-limiting guide that can be assembled and inserted quickly. It also provides increased surgical assistance by guiding the 2-mm twist drill of adjacent implants, ensuring parallelism, symmetry, and uniform implant spacing from the midline. Upon creation of the osteotomy with the 2-mm twist drill to the final depth, the guide is removed and the osteotomy expanded to the desired diameter without it. Because the guide is minimally obtrusive, it allows complete visualization of the surgical field and does not limit irrigant from reaching the osteotomy, which is a potential drawback of computer-generated, fully limited guides.27
Expanding on the work of McArthur, who determined an average size ratio between maxillary and mandibular incisors, Wheeler presented the ideal mesiodistal dimensions of the 32 natural permanent teeth.22,23 The 5 mm, 7 mm, 9 mm combination of interimplant distance used in the FLIP guide is based on the interdental distance between adjacent natural teeth. Creating adjacent osteotomies spaced at 5 mm between mandibular anterior teeth, 7 mm between mandibular premolars or between premolars and molars, and 9 mm between mandibular molars allows for implants to be placed at an ideal distance from each other while also respecting the optimal natural tooth positions (Figure 1).
Conclusion
The FLIP guide was used in the three cases shown to aid in achieving parallelism and symmetry of the implants. This guide, which may be utilized as an alternative to a conventional, duplicated denture-based guide, provided exceptional surgical accuracy through its ability to be secured to the ridge and guide the initial implant drills. The minimally obtrusive guide can be quickly assembled chairside and easily adapted to the shape of the dental arch. Also, it interferes only minimally with irrigation solution. The resulting parallelism allows for the use of maximum-strength retentive components and ease of insertion and removal of the overdenture. In the full-arch implant case presented, the 5 mm, 7 mm, 9 mm combination of interimplant spacing in the FLIP guide was beneficial, as the parallelism allowed for a full-arch restoration with screw-access holes located at positions corresponding to ideal tooth dimensions. Furthermore, the versatility of the guide may enable its use in partially edentulous situations, such as multiple missing adjacent mandibular anterior teeth.
Acknowledgment
The authors thank Jacqueline Eriguel, DMD, for her assistance in finalizing the manuscript.
Disclosure
The authors had no disclosures or conflicts of interests to report with regard to any of the materials or companies mentioned in this article.
About the Authors
Shalin Vinayak, DMD, MFD
Resident, Ashman Department of Periodontology and Implant Dentistry, New York University College of Dentistry, New York, New York; Private Practice, Nairobi, Kenya
Stuart J. Froum, DDS
Clinical Adjunct Professor and Director of Clinical Research, Ashman Department of Periodontology and Implant Dentistry, New York University College of Dentistry, New York; Private Practice, New York, New York
Kuanyou Liu, DDS
Former Resident, Ashman Department of Periodontology and Implant Dentistry, New York University College of Dentistry, New York, New York; Private Practice, Taiwan
Anna Corinna Lim, DDS
Former Resident, Ashman Department of Periodontology and Implant Dentistry, New York University College of Dentistry, New York, New York; Private Practice, Tacoma, Washington
Michael Liang, DDS
Resident, Ashman Department of Periodontology and Implant Dentistry, New York University College of Dentistry, New York, New York
References
1. Doundoulakis JH, Eckert SE, Lindquist CC, Jeffcoat MK. The implant-supported overdenture as an alternative to the complete mandibular denture. J Am Dent Assoc. 2003;134(11):1455-1458.
2. Feine JS, Carlsson GE, Awad MA, et al. The McGill consensus statement on overdentures. Mandibular two-implant overdentures as first choice standard of care for edentulous patients. Montreal, Quebec, May 25-25, 2002. Int J Oral Maxillofac Implants. 2002;17(4):601-602.
3. Schnitman PA, Wöhrle PS, Rubenstein JE, et al. Ten-year results for Brånemark implants immediately loaded with fixed prostheses at implant placement. Int J Oral Maxillofac Implants. 1997;12(4):495-503.
4. Balshi TJ, Wolfinger GJ. Immediate loading of Brånemark implants in edentulous mandibles: a preliminary report. Implant Dent. 1997;6(2):83-88.
5. Drago CJ. Prosthodontic complications related to compromised implant placement. J Oral Maxillofac Surg. 1994;52(1):15-22.
6. Memari Y, Geramy A, Fayaz A, et al. Influence of implant position on stress distribution in implant-assisted distal extension removable partial dentures: a 3D finite element analysis. J Dent (Tehran). 2014;11
(5):523-530.
7. Rojas-Vizcaya F. Biological aspects as a rule for single implant placement. The 3A-2B rule: a clinical report. J Prosthodont. 2013;22(7):575-580.
8. Funato A, Salama MA, Ishikawa T, et al. Timing, positioning, and sequential staging in esthetic implant therapy: a four-dimensional perspective. Int J Periodontics Restorative Dent. 2007;27(4):313-323.
9. Esposito M, Ekestubbe A, Gröndahl K. Radiological evaluation of marginal bone loss at tooth surfaces facing single Brånemark implants. Clin Oral Implants Res. 1993;4(3):151-157.
10. Spray JR, Black CG, Morris HF, Ochi S. The influence of bone thickness on facial marginal bone response: stage 1 placement through stage 2 uncovering. Ann Periodontol. 2000;5(1):119-128.
11. Tarnow DP, Cho SC, Wallace SS. The effect of inter-implant distance on the height of inter-implant bone crest. J Periodontol. 2000;71(4):546-549.
12. Grunder U, Gracis S, Capelli M. Influence of the 3-D bone-to-implant relationship on esthetics. Int J Periodontics Restorative Dent. 2005;25(2):113-119.
13. Salama H, Salama MA, Garber D, Adar P. The interproximal height of bone: a guidepost to predictable aesthetic strategies and soft tissue contours in anterior tooth replacement. Pract Periodontics Aesthet Dent. 1998;10(9):1131-1141.
14. Ishikawa T, Salama H, Funato A, et al. Three-dimensional bone and soft tissue requirements for optimizing esthetic results in compromised cases with multiple implants. Int J Periodontics Restorative Dent. 2010;30(5):503-511.
15. Buser D, Martin W, Belser UC. Optimizing esthetics for implant restorations in the anterior maxilla: anatomic and surgical considerations. Int J Oral Maxillofac Implants. 2004;19 suppl;43-61.
16. Weinberg LA. Tooth position in relation to the denture base foundation. J Prosthet Dent. 1958;8(3):398-405.
17. Misch CE. Contemporary Implant Dentistry. 3rd ed. St. Louis, MO: Mosby Elsevier; 2008.
18. Nickenig HJ, Eitner S, Rothamel D, et al. Possibilities and limitations of implant placement by virtual planning data and surgical guide templates. Int J Comput Dent. 2012;15(1):9-21.
19. Nickenig HJ, Spiekermann H. CT-based surgical templates vs. traditional surgical guides. J Dent Implant. 2006;22:272-280.
20. Rußig LL, Schulze RK. Effects of minute misregistrations of prefabricated markers for image-guided dental implant surgery: an analytical evaluation. Clin Oral Implants Res. 2013;24(12):1339-1346.
21. Misir AF, Sumer M, Yenisey M, Ergioglu E. Effect of surgical drill guide on heat generated from implant drilling. J Oral Maxillofac Surg. 2009;67(12):2663-2668.
22. Van Assche N, Vercruyssen M, Coucke W, et al. Accuracy of computer-aided implant placement. Clin Oral Implants Res. 2012;23 suppl 6:112-123.
23. Nelson SJ. Wheeler's Dental Anatomy, Physiology, and Occlusion. 10th ed. Elsevier Health Sciences; 2014.
24. Gulizio MP, Agar JR, Kelly JR, Taylor TD. Effect of implant angulation upon retention of overdenture attachments. J Prosthodont. 2005;14(1):3-11.
25. Thomason JM, Kelly SA, Bendkowski A, Ellis JS. Two implant retained overdentures-a review of the literature supporting the McGill and York consensus statements. J Dent. 2012;40(1):22-34.
26. Selim K, Ali S, Reda A. Implant supported fixed restorations versus implant supported removable overdentures: a systematic review. Open Access Maced J Med Sci. 2016;4(4):726-732.
27. Misir AF, Sumer M, Yenisey M, Ergioglu E. Effect of surgical drill guide on heat generated from implant drilling. J Oral Maxillofac Surg. 2009;67(12):2663-2668.