Improving the Esthetics of Single Tooth Implant Restorations in the Anterior Maxilla
Use of a diagnostic guide enables prosthetic information to be incorporated into virtual implant planning and the design of the surgical guide
Sean W. Meitner, DDS, MS | Gregori M. Kurtzman, DDS
Implant placement to replace a single tooth, whether immediately following extraction or at a site that has undergone extraction but been given time to heal, can pose challenges related to the osseous anatomy and the adjacent teeth.1 These challenges can become more significant in the maxillary anterior region, particularly when the angulation of the premaxilla requires the implant to be placed at an angle (ie, axis) that is different from the prosthetic axis required to restore it with proper esthetics.2 In addition, concavities on the facial aspect of the ridge may require the placement of osseous graft materials to ensure that the implant is completely encased within the bone and that no dehiscence is present.
The use of a surgical guide can aid in the placement of implants within the osseous anatomy in ideal positions that respect the adjacent teeth and anatomical structures (eg, nasal fossa, incisive fossa, incisive nerve, etc). Furthermore, virtual planning can aid in the fabrication of more accurate surgical guides, which is especially relevant considering that the anatomical structures to be respected are not visible to the naked eye during surgery. Although virtual planning permits consideration of these anatomical structures, it typically does not provide prosthetic information. Implant placement should be prosthetically driven so that the implants' platforms are in ideal positions for the restorations to be designed to not only be functional but also esthetically blend with the adjacent natural teeth.3 Therefore, prosthetic information should be incorporated into the planning phase.4 This can be achieved by using a diagnostic guide during acquisition of the cone-beam computed tomography (CBCT) scan. With a diagnostic guide representing the ideal prosthetic axis, the virtual position of the implant can be idealized in the planning software and used to create a more accurate surgical guide. The diagnostic guide and surgical guide can be fabricated in-office, which eliminates the time delays that are associated with having a laboratory fabricate them and lowers the costs of fabrication.5 The following case report demonstrates the use of a diagnostic guide to improve implant planning and the creation of a surgical guide for the restoration of a failing maxillary anterior tooth that required osseous grafting prior to implant placement.
Case Report
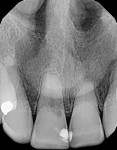
A 58-year-old female patient was referred to the practice because she was experiencing sensitivity associated with her maxillary right central incisor. A periapical radiograph was acquired, which demonstrated that the tooth had undergone external cervical resorption (Figure 1). The patient was informed that the tooth had a poor prognosis and presented with two treatment options: extraction followed by the placement of a conventional 3-unit bridge or extraction followed by the placement of an implant-supported restoration. Because the patient did not want to have the adjacent teeth prepared for a bridge, she chose the implant treatment option. An impression was then acquired to fabricate an Essix® temporary prosthesis for the patient to use following extraction.
Extraction and Diagnostic Guide Fabrication
The patient presented for treatment and reviewed and signed the consent form. After a local anesthetic was administered via infiltration into the buccal vestibule, an elevator was used to luxate the tooth, and then, it was extracted atraumatically with forceps. At this time, a concavity was noted on the buccal aspect of the ridge at the extraction site, which indicated that bone grafting may be required for implant placement (Figure 2).
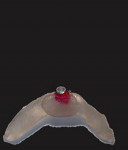
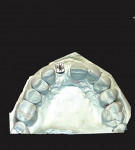
Following extraction, impressions were acquired, and a cast was created. Fabrication of the diagnostic guide was initiated by creating a pilot hole in the cast at the extraction site using a 3/32" drill positioned in an ideal prosthetic position and angle centered between the adjacent lateral and central incisors (Figure 3). Next, a 3-mm guide post (Guide Right™, DePlaque) was inserted into the hole in the cast, and a 3-mm guide sleeve (Guide Right™, DePlaque) was placed over the post with the retention cleat positioned at the lingual aspect (Figure 4). Modeling resin (Primopattern LC Gel, Primotec USA) was placed on the guide sleeve cleat to stabilize the guide sleeve (Figure 5), and then additional resin was placed onto the occlusal/incisal surfaces of the adjacent teeth and light-cured to complete the diagnostic guide (Figure 6). The patient returned to the office, and after the diagnostic guide was tried in to ensure a stable fit, a CBCT scan was acquired to initiate the virtual planning. The temporary prosthesis was then delivered, and the patient was scheduled for a surgical appointment.
Initial Implant Planning
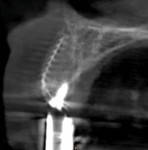
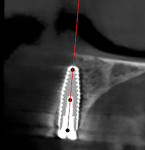
The CBCT scan was imported into planning software (CS 3D Imaging Software, Carestream Dental). In the software, a virtual implant was placed from a prosthetic standpoint using a long axis through the guide sleeve of the diagnostic guide in the image. A 10° angle correction and a 1-mm linear correction would be required based on the anatomy present. In addition, the cross-sectional view indicated that osseous graft material would be needed to create sufficient volume to house the planned implant (Figure 7). Due to the volume of missing bone on the buccal ridge, osseous grafting would need to be performed and the area would need to be allowed to heal prior to implant placement. In preparation for the grafting procedure, a piece of titanium mesh (Ti-Mesh, Impladent Ltd) was cut and shaped to fit the edentulous area on the cast (Figure 8).
Bone Grafting
When the patient returned for the surgical appointment, consent forms were reviewed and signed, and a local anesthetic was administered. A resorbable mineralized collagen bone graft material (OsteoGen® Strip, Impladent Ltd) was wetted with a 50 µg recombinant human bone morphogenetic protein-2 solution (Infuse®, Medtronic) and allowed to set for 15 minutes prior to placement. To begin the procedure, a scalpel was used to make an incision in the buccal sulcus from the distal aspect of the left central incisor to the distal aspect of the right canine across the papillae, and a full-thickness flap was elevated without vertical releasing incisions to fully expose the buccal ridge defect. The previously prepared graft material was then placed at the defect and the titanium mesh was placed over it and fixated to the crest of the ridge with a screw (Figure 9). Tension-free primary closure was achieved by fixating the flap with sutures (Figure 10). The Essix retainer was reinserted to continue as a provisional prosthesis, and the patient was scheduled for recall appointments.
When the patient was seen 4 months after graft placement to evaluate the clinical results, the prior defect had been eliminated and the ridge demonstrated a natural facial contour (Figure 11). The diagnostic guide was placed intraorally once again, and another CBCT scan was acquired to evaluate the new osseous dimensions, complete the final implant planning from a prosthetically-driven approach, and produce the surgical guide (Figure 12). The patient was scheduled for the implant placement appointment and dismissed.
Final Planning and Surgical Guide Fabrication
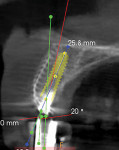
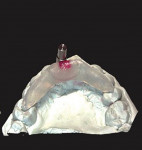
The titanium mesh could be visualized on the CBCT scan, and an improved ridge contour was evident as outlined by the mesh in the cross-sectional view. The planned 4.1 × 12 mm bone-level implant (Roxolid® SLActive®, Straumann) was virtually positioned in the cross-sectional view to be within the osseous contours of the ridge (Figure 13). As indicated by the initial virtual planning prior to graft placement, a 10° angle correction and a 1-mm linear correction would be required. To fabricate the surgical guide, a 1-mm offset guide post (Guide Right™, DePlaque) was placed into the post hole on the cast (Figure 14), followed by a 3.9 mm upper removable part and a 3.9 mm guide sleeve (Figure 15). Modeling resin was then added to stabilize the guide sleeve, and additional resin was added to complete the surgical guide (Figure 16).
Implant Placement
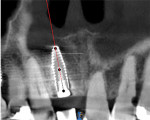
On the day of implant placement, the consent form was reviewed and signed, and a local anesthetic was administered. Using the same approach that was used to expose the ridge for grafting, an incision was made, and a full-thickness flap was elevated to permit visualization of the previously placed titanium mesh (Figure 17). The fixation screw at the crest's peak was removed, followed by the titanium mesh, revealing a wider osseous ridge for implant placement. The prosthetically informed surgical guide was then inserted intraorally, and its fit and stability were verified. Next, 3.9-mm, 2° tapered depth stop drills (Guide Right™, DePlaque) were introduced though the sleeve on the surgical guide until the planned depth was reached (Figure 18 and Figure 19). The final osteotomy preparation was performed through the surgical guide utilizing a drill (Straumann® Guided Surgery Instruments, Straumann) with a diameter matching that of the planned implant (Figure 20). To achieve subcrestal placement of the implant's platform, the depth of the osteotomy was increased following removal of the surgical guide, and then the implant was placed (Figure 21). A cover screw was placed on the implant, and the soft tissue was sutured closed. Following implant placement, a CBCT scan was acquired to document the implant's position in relation to the adjacent teeth and surrounding anatomy (Figures 22 and Figure 23). The patient continued to use the Essix retainer as a provisional prosthesis during the integration period.
Final Restoration
Following a 4-month healing and integration period, the patient returned to the practice. The implant was uncovered, and the cover screw was replaced with a healing abutment. The implant's Implant Stability Quotient score was determined to be 75; therefore, the patient was scheduled to see the restoring dentist 2 weeks later to initiate the restorative phase of treatment. The Essix retainer was modified to seat over the healing abutment without any contact so that it could continue to serve as a provisional prosthesis.
At the appointment with the restoring dentist, the healing abutment was removed, an implant impression abutment was placed, and impressions were acquired for the planned crown. The healing abutment was then reinserted. Next, a shade was selected to blend with the adjacent teeth, and the shade information was sent to the laboratory along with the impressions for the fabrication of a custom abutment and the final crown.
The patient returned, and the final restoration was placed. Esthetically, it blended excellently with the adjacent natural dentition (Figure 24). A periapical radiograph was acquired to confirm the full seating of the restoration to the implant at the platform (Figure 25). In addition, the occlusion was checked, which revealed very light contact on the lingual of the implant restoration, so no adjustments were needed.
Conclusion
Implant placement for a single tooth restoration in the maxillary anterior region can present clinical challenges. These include anatomical challenges related to the angulation of the premaxilla and potential osseous defects on the buccal aspect of the crest. Virtual planning and the use of a surgical guide help to eliminate problems that can occur when a freehand surgical approach is followed. Because implant placement should be prosthetically driven, especially in the esthetic zone, the use of a diagnostic guide during the acquisition of the initial CBCT scan to incorporate prosthetic information can improve virtual planning and enable the fabrication of surgical guides that facilitate more ideal implant placement. This can become more critical when osseous augmentation is required to create a site that can accommodate the planned implant. Beyond improved accuracy, in-office creation of the diagnostic guide and surgical guide eliminates laboratory fees and shortens the time between consultations and surgical appointments.
About the Author
Sean W. Meitner, DDS, MS
Diplomate, American Academy of Periodontology
Associate Professor, Department of Periodontology
Eastman Institute for Oral Health
University of Rochester
Rochester, New York
Private Practice
Fairport, New York
Gregori M. Kurtzman, DDS
Master, Academy of General Dentistry
Diplomate, International Congress of Oral Implantologists
Private Practice
Silver Spring, Maryland
References
1. Pimkhaokham A, Jiaranuchart S, Kaboosaya B, et al. Can computer-assisted implant surgery improve clinical outcomes and reduce the frequency and intensity of complications in implant dentistry? A critical review. Periodontol 2000. 2022;90(1):197-223.
2. Chen ST, Buser D, Sculean A, Belser UC. Complications and treatment errors in implant positioning in the aesthetic zone: Diagnosis and possible solutions. Periodontol 2000. 2023;92(1):220-234.
3. D'haese J, Ackhurst J, Wismeijer D, et al. Current state of the art of computer-guided implant surgery. Periodontol 2000. 2017;73(1):121-133.
4. Morton D, Phasuk K, Polido WD, Lin WS. Consideration for contemporary implant surgery. Dent Clin North Am. 2019;63(2):309-329.
5. Meitner S, Phillips S, Carneiro L, et al. Evaluation of the accuracy of a new geometric approach to implant guidance. Int J Oral Maxillofac Implants. 2022;37(1):104-113.