Full-Mouth Rehabilitation With Fixed Full-Arch Zirconia Prostheses
Low-speed osteotomy preparation without irrigation improves bone health at implant sites for optimal outcomes
Enrico Luigi Agliardi, MD, DDS | Stefano Panigatti, MD, DDS | Giulia Moreo, DDS | Irene Cusenza, DDS Jacopo Agliardi | Davide Romeo, DDS, MS, PhD
Nowadays, delivering immediate full-arch, fixed implant-supported prostheses can be considered a predictable treatment for both jaws, and it is associated with high levels of patient satisfaction in terms of function, phonetics, and esthetics.1-3 The original protocol proposed by Brånemark4 has been substantially modified in many aspects, particularly with the development of new implant morphologies and restorative materials and the introduction of innovative surgical and prosthetic workflows.
Osseointegration is influenced by implant geometry and microdesign, bone morphology, and surgical drilling protocols and speed.5 In this regard, research has shown that low-speed drilling can prevent bone necrosis during implant site preparation because areas of necrotic bone around implants are associated with drill-induced heat that is proportional to rotational speed.6,7 Implant systems have been introduced that are designed to protect the biology of the surgical site by using a low-speed drilling protocol with no irrigation.8,9 The following case report illustrates a full-arch immediate implant rehabilitation using such an implant system and the All-on-4® treatment concept10,11 with approximately 5 years of follow-up. The definitive prostheses were fabricated in full zirconia without metal connectors following a digital workflow.
Case Report
A 63-year-old female patient presented for an initial consultation, at which time she reported that many of her residual teeth exhibited mobility and that her masticatory function was compromised. Her chief complaint was that she wanted to achieve better occlusion and improve the esthetics of her smile with fixed dental prostheses; however, she wanted to avoid receiving removable restorations if possible. The clinical examination evidenced partial edentulism in both arches as well as malpositioned teeth and revealed that the patient's maxillary anterior teeth were in excessive contact with the vermilion of her lower lip during maximum smile (Figure 1 and Figure 2). In addition, clinical attachment loss with localized probing depths greater than 3 mm, soft-tissue recession, and clinical mobility, particularly among the mandibular teeth, were noted. Evaluation of a panoramic radiograph (Figure 3) and a cone-beam computed tomography (CBCT) scan indicated bilateral pneumatization of the maxillary sinus cavities and generalized horizontal bone resorption.
The long-term prognosis of the majority of the patient's residual teeth was unfavorable. Therefore, the proposed treatment involved the placement of axial and tilted implants in each arch that would be immediately loaded with fixed full-arch dental prostheses (ie, All-on-4 protocol). The patient agreed to treatment and signed an informed consent form. Clinical photographs and intraoral scans (TRIOS® 3, 3Shape) were acquired at the current vertical dimension of occlusion for the fabrication of study models, and then temporary dentures were fabricated for chairside conversion and immediate loading.
Implant Placement and Immediate Loading
Both of the patient's arches were treated on the same day. A 0.2% chlorhexidine digluconate mouthwash (Curasept® ADS, Curasept S.p.A.) was prescribed to the patient for daily rinses, which were initiated 3 days prior to surgery and then continued for 7 days following surgery. One hour prior to surgery, a dose of 2 g of amoxicillin and clavulanic acid (Augmentin®, Roche) was administered to the patient for antibiotic prophylaxis. The surgery was performed under intravenous sedation (5 mg of diazepam), and a corticosteroid (4 mg dexamethasone), anti-inflammatory agent (30 mg ketorolac tromethamine), and anti-acid medication (50 mg ranitidine) were administered during the procedure.
After local anesthesia was achieved with articaine chlorhydrate 4% and adrenaline 1:100,000 (Alfacaina N, Weimer Pharma), the patient's remaining teeth were extracted, and the sockets were carefully debrided. For the treatment of each arch, a midcrestal incision was made, equally dividing the available keratinized gingiva, followed by two posterior vertical releasing incisions, which enabled the careful elevation of buccal and lingual/palatal full thickness flaps. The mental nerve was isolated, and the extension of the anterior loop, if present, was estimated with the use of an atraumatic periodontal probe gently placed into the canals. Following elevation of the flaps, the crest was regularized with bony forceps and rotary instruments to create a flap surface for better soft-tissue adaptation.
Once the crest was regularized, the osteotomies were prepared using two sequential drills that were specifically designed for the low-speed drilling protocol of the chosen implant system (N1™ Implant System, Nobel Biocare). The first drill (OsseoDirector™, Nobel Biocare), which has side-cutting ability, was used at ≤ 2,000 rpm with saline irrigation to establish the position, angle, and depth of the osteotomies (Figure 4). The second drill (OsseoShaper™, Nobel Biocare) was then used at 50 rpm (and with a maximum torque of 40 Ncm) without irrigation to complete the osteotomies (Figure 5). Next, while avoiding irrigation of the surgical sites, the implants (N1™ Implant, Nobel Biocare) were placed using a surgical handpiece. These implants have a tri-oval tapered shape that results in the formation of high strain areas for stability and low strain areas where osteogenic potential is preserved, which leads to secondary stability.12 Four implants were placed in each arch: two anterior axial implants in the positions of the lateral incisors and two posterior tilted implants at the sites of the second premolars. The posterior implants were inserted with a mesiodistal inclination of approximately 30°, respecting the integrity of the mental nerve and the sinus cavities. All of the implants were 4 mm in diameter and 13 mm in length, and they all achieved a minimum insertion torque of 40 Ncm (Figure 6).
Following implant placement, multi-unit abutments (N1™ Multi-Unit Abutments, Nobel Biocare) were inserted. Abutments with a 30° angulation were positioned on the distal implants to obtain an optimal orientation for the prosthetic screws. For the anterior implants, straight abutments were placed over the mandibular ones, and abutments with a 17° angulation were connected over the maxillary implants (Figure 7). The soft tissues were then sutured closed. Next, titanium cylinders were screwed over the abutments, and the immediate dentures were converted chairside into full acrylic fixed prostheses containing 10 teeth each. The cantilevers were removed, and light contacts in maximum intercuspation were established. After the access holes were sealed with PTFE tape and flowable composite (Figure 8), panoramic and periapical radiographs were acquired to verify the seating of the prosthetic components (Figure 9). The temporary prostheses would be used to assess the patient's esthetics, phonetics, and masticatory function as well as her ability to maintain proper oral hygiene (Figure 10). The patient was sent home with the recommendation to maintain a diet of soft foods for the first 3 months after surgery.
Delivery of the Definitive Prostheses
After a 4-month healing period needed for osseointegration and maturation of the peri-implant soft tissue (Figure 11 through Figure 13), the patient decided to move forward with the fabrication of the definitive prostheses. A double digital scanning protocol was followed, and the patient was scheduled for final records. During the first appointment, an intraoral scan was acquired with the immediate prostheses in place to capture both prostheses and the occlusion (Figure 14). Subsequently, the temporary prostheses were removed, scan bodies were manually tightened over the multi-unit abutments, and another intraoral scan was acquired to record the 3D position of the implants (Figure 15).
The digital STL files were then imported into CAD software (Exocad DentalCAD®, Exocad GmbH) for the design of verification indexes (Figure 16) and esthetic prototypes. Those jigs were milled in aluminum, and during the second appointment, they were placed intraorally for a clinical verification of fit using the Sheffield test (Figure 17 and Figure 18). For this test, one screw was torqued in at one end of each index, and their fit was assessed clinically and radiographically (Figure 19) by a prosthodontist with experience with full-arch prostheses. Visible gaps were noted at the contralateral abutments; therefore, the indexes were judged to not have a passive fit. As a result, both indexes were sectioned into various segments, splinted intraorally with low-shrinkage acrylic resin (Pattern Resin™ LS, GC America), and finally removed from the mouth with a pick-up impression. Physical casts were then made.
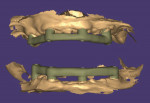
Next, the prototypes were milled from a PMMA disc (Figure 20), tried in the patient's mouth to assess function, phonetics, and esthetics (Figure 21), and then scanned with a desktop scanner to finalize the design of the final prostheses (Figure 22). Occlusal adjustments were made, and the patient provided feedback regarding any desired esthetic changes before the fabrication of the final all-zirconia prostheses. The adjusted prototypes were then scanned in the laboratory, and the final full-arch, monolithic full-contour zirconia (NobelProcera® Zirconia Implant Bridge [Nacera® Pearl], Nobel Biocare) prostheses without metal components were fabricated (Figure 23 and Figure 24). To further personalize the esthetics, feldspathic porcelain was applied to the facial surfaces of the teeth.
The final zirconia prostheses were delivered during a third appointment (Figure 25 through Figure 29). At this time, the prosthetic screws were torqued to 15 Ncm, the occlusion was checked, and the screw access holes were sealed with PTFE tape and flowable composite. A panoramic radiograph was then acquired for final verification (Figure 30).
Ongoing Hygiene and Follow-Up
Following delivery of the definitive prostheses, the patient was scheduled to return to the practice three times a year for professional oral hygiene sessions. After approximately 5 years of follow-up, all of the implants remained stable, and none of them registered marginal bone remodeling greater than 2 mm. No mechanical or technical complications were recorded with either the temporary or definitive prostheses.
Conclusion
This case report illustrates a simplified and effective protocol for the full-mouth rehabilitation of patients using a digital workflow to deliver passive definitive full-arch zirconia prostheses. Because acquiring intraoral scans for full-arch digital implant cases can be very challenging, the accuracy of the scans should be evaluated through a verification index or other method to provide quality control. The implant system selected for this case resulted in the creation of osteotomies with low heat generation and minimal invasiveness when compared with traditional drilling protocols, thus preserving the vitality of the bone for optimal results.
About the Authors
Enrico Luigi Agliardi, MD, DDS
Associate Professor
Department of Dentistry
Vita Salute University
San Raffaele Hospital
Milan, Italy
Stefano Panigatti, MD, DDS
Adjunct Professor
Department of Dentistry
Vita Salute University
San Raffaele Hospital
Milan, Italy
Giulia Moreo, DDS
Postgraduate Resident
Department of Dentistry
Vita Salute University
San Raffaele Hospital
Milan, Italy
Irene Cusenza, DDS
Postgraduate Resident
Department of Dentistry
Vita Salute University
San Raffaele Hospital
Milan, Italy
Jacopo Agliardi
Dental Student
Department of Dentistry
Vita Salute University
San Raffaele Hospital
Milan, Italy
Davide Romeo,DDS, MS, PhD
Adjunct Professor
Department of Dentistry
Vita Salute University
San Raffaele Hospital
Milan, Italy
References
1. Gallardo YNR, da Silva-Olivio IR, Gonzaga L, et al. A systematic review of clinical outcomes on patients rehabilitated with complete-arch fixed implant-supported prostheses according to the time of loading. J Prosthodont. 2019;28(9):958-968.
2. Jiang X, Zhou W, Wu Y, Wang F. Clinical outcomes of immediate implant loading with fixed prostheses in edentulous maxillae: a systematic review. Int J Oral Maxillofac Implants. 2021;36(3):503-519.
3. Gonçalves GSY, de Magalhães KMF, Rocha EP, et al. Oral health-related quality of life and satisfaction in edentulous patients rehabilitated with implant- supported full dentures all-on-four concept: a systematic review. Clin Oral Investig. 2022;26(1):83-94.
4. Brånemark PI, Hansson BO, Adell R, et al. Osseointegrated implants in the treatment of the edentulous jaw. Experience from a 10-year period. Scand J Plast Reconstr Surg Suppl.1997;16:1-132.
5. Coelho PG, Jimbo R. Osseointegration of metallic devices: current trends based on implant hardware design. Arch Biochem Biophys. 2014;561:99-108.
6. Giro G, Marin C, Granato R, et al. Effect of drilling technique on the early integration of plateau root form endosteal implants: an experimental study in dogs. J Oral Maxillofac Surg. 2011;69(8):2158-2163.
7. Möhlhenrich SC, Modabber A, Steiner T, et al. Heat generation and drill wear during dental implant site preparation: systematic review. Br J Oral Maxillofac Surg. 2015;53(8):679-689.
8. Meljon A, Geisendorf M, Kamber S, et al. Evaluation of heat generated by a new site preparation using low-speed tools without irrigation. Clin. Oral Impl. Res. 2021;32(S22):111.
9. Fabbri G, Staas T, Urban I. A retrospective observational study assessing the clinical outcomes of a novel implant system with low-speed site preparation protocol and tri-oval implant geometry. J Clin Med. 2022;11(16):4859.
10. Maló P, Rangert B, Nobre M. "All-on-Four" immediate-function concept with Brånemark System implants for completely edentulous mandibles: a retrospective clinical study. Clin Implant Dent Relat Res. 2003;5(Suppl 1):2-9.
11. Agliardi EL, Pozzi A, Romeo D, Del Fabbro M. Clinical outcomes of full-arch immediate fixed prostheses supported by two axial and two tilted implants: A retrospective cohort study with 12-15 years of follow-up. Clin Oral Implants Res. 2023;34(4):351-366.
12. Yin X, Li J, Hoffmann W, et al. Mechanical and biological advantages of a tri-oval implant design. J Clin Med. 2019;8(4):427.