Incidental CBCT Findings: The Importance of Reading the Whole Image
Jenna Zhu, DMD; Brooke Blicher, DMD; and Rebekah Lucier Pryles, DMD
Abstract: The use of cone-beam computed tomography (CBCT) imaging often elicits changes in both diagnostics and treatment plans when incorporated into endodontic workups. In endodontic practice, CBCT scans enable detection of periapical pathology before it is apparent on traditional 2-dimensional intraoral radiographs. The visualization provided by CBCT scans can help clinicians confirm suspected diagnoses, including but not limited to periapical pathology, traumatic tooth displacement, and vertical root fracture. This article discusses the use of CBCT imaging in the field of endodontics with an emphasis on its utilization to identify incidental findings, which can introduce complexities to a diagnosis and yield valuable information to enhance the scope of care for the patient.
Cone-beam computed tomography (CBCT) has revolutionized the practice of endodontics. Such images are useful across the full spectrum of this dental specialty, from diagnosis to treatment planning, delivery of care, and follow-up. The evidence is clear that CBCT imaging often prompts changes in both diagnostics and treatment plans when incorporated into endodontic workups,resulting in its frequent adoption into endodontic specialty practice.1
While the area of focus in endodontics typically is the pathology surrounding the tooth and its proximal structures, the ordering practitioner is responsible for interpretation of the entirety of the scanned area.2 According to multiple studies, more than 90% of large field-of-view (FOV) CBCT scans have incidental findings.3-6 In the field of endodontics, practitioners primarily use limited FOV CBCT scans. However, despite their frequent utilization in practice, there are few studies on the rates of incidental findings found in limited FOV CBCT scans used in endodontics.7
CBCT's Usefulness in Endodontic Practice
In 2015, the American Association of Endodontists and the American Academy of Oral and Maxillofacial Radiology updated their joint position statement guiding clinicians on case selection for use of CBCT in endodontic practice.2 In the diagnosis phase, limited FOV CBCT scans are recommended for diagnosis in patients who present with contradictory or nonspecific clinical signs and symptoms, especially when clinical and radiographic examinations are inconclusive.2 CBCT scans are able to detect periapical pathology before it is apparent on traditional 2-dimensional radiographs.7 Visualization from CBCT scans as opposed to intraoral radiographs can oftentimes help clinicians confirm suspected diagnoses ranging from periapical pathology to traumatic tooth displacement and even vertical root fracture.2
Preoperatively, CBCT scans can also provide valuable information about teeth with the potential for extra canals, suspected complex morphology, and dental anomalies.2 In addition, during treatment, these scans can help identify and localize calcified canals so clinicians can make informed decisions on how to proceed in their treatment sequence. After treatment, if there is a lack of healing within the appropriate timeframe, CBCTs can help clinicians assess for any previous nonsurgical treatment complications, allowing them to make a clinical judgment on whether the tooth should undergo nonsurgical retreatment, surgical treatment, or extraction.2
CBCT images are recommended in the workup of traumatic dental injuries, particularly when root fractures are suspected, and for cases of resorption or fractured teeth.2 Like most imaging modalities used in dentistry, limited FOV CBCT scans still produce low amounts of ionizing radiation and should be used with consideration of "as low as reasonably achievable (ALARA)" principles or the newer "as low as diagnostically acceptable (ALADA)" principles.2
Given its utility in diagnosis, treatment, and follow-up, CBCT imaging has seen routine adoption in the field of endodontics. As previously stated, incidental findings are not uncommon in scan volumes and may go undetected without careful inspection of the images. In a study by Oser et al, the prevalence of undetected incidental findings in limited FOV CBCT scans was compared between a medical radiologist and an endodontic resident.8 The radiologist reported a significantly greater number of abnormalities (87%) in the 203 scans evaluated compared to the endodontic resident (50%). Langella et al did a study in which those same 203 scans were reviewed and evaluated by endodontic residents while additionally using a checklist during the review.9 The incidental findings checklist included: rarefying osteitis, sinusitis/mucosal lining thickening, excess restorative material in periapical area, mucous retention pseudocysts, impactions, root resorptions - external or internal, sclerosing osteitis, nasopalatine duct cyst, retained root tips, idiopathic osteosclerosis/enostosis, cemento-osseous dysplasia, fibrous dysplasia, other.9 From this study, the endodontic residents reported an increased number of abnormalities (91%) compared to the resident in the previous study but also an increased number of false positive findings. This study illustrated that the use of a checklist when interpreting limited FOV CBCT scans can improve the rate of identification of common incidental findings. In another study, by Rai et al, 89% of subjects showed incidental findings on their CBCT scans.10
Analyzing Incidental Findings
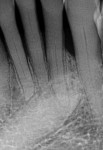
Although checklists can be useful in research and in training providers to be aware of incidental findings, ordering clinicians, as previously mentioned, are responsible for reading any and all structures in an exposed image, including normal and abnormal findings that warrant additional diagnosis or treatment. Upon review of CBCT scans, providers may come across findings separate from the endodontic issue in question (Figure 1). With regard to the suspected tooth with pathology, the CBCT scan may reveal caries, fractures, resorption, or non-endodontic pathology. Because even limited FOV scan volumes include multiple teeth, other odontogenic pathology can be noted on adjacent teeth. Incidental findings may also include cysts and tumors, such as odontomas, dentigerous cysts, and cemento-osseous conditions. Maxillary sinus findings are among the most common incidental findings, and include mucositis, mucous retention cysts, and calcifications, among others.10 Other findings in soft tissues can include sialoliths within salivary glands. In addition, when large FOV images are utilized, incidental findings may occur in visualized extragnathic regions, such as the airway or brain. It is crucial that the clinician meticulously analyzes each scan to its full extent to avoid missing any critical pieces of information.2
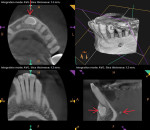
Figure 2 and Figure 3 demonstrate common incidental findings in limited FOV scans. In this case, the patient was sent to an endodontics specialty office because the hygienist reported a fistula in the anterior mandible. Upon diagnostic evaluation by the endodontist, no sinus tracts were visible and all endodontic testing was normal. However, a limited FOV CBCT scan revealed an impacted canine with evidence of pre-eruptive resorption positioned in the facial bone adjacent to mandibular incisors, as well as a sialolith as incidental findings. There was, in fact, no evidence of endodontic pathosis. As a result, referral was made to an oral and maxillofacial surgeon (OMFS) for the workup of both issues.
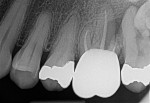
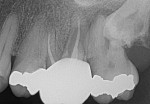
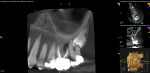
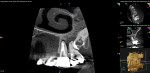
In the case presented in Figure 4 through Figure 7, incidental findings were discovered because of the limited FOV scan. The patient was seen for intermittent and poorly localized discomfort. The periapical radiographs illustrated apical periodontitis, the most commonly radiographically visible endodontic pathology, which was centered on tooth No. 15 (Figure 4 and Figure 5). The CBCT scan, however, further unfolded the true extension of pathology, including the apices of tooth No. 14 and the adjacent impacted tooth No. 16, as well as evidence of pressure resorption affecting tooth No. 15, intracoronal resorption associated with tooth No. 16, and generalized mucositis in the adjacent maxillary sinus (Figure 6 and Figure 7). The scope of symptomatic disease in the patient was fully visualized, and the treatment plan included endodontic retreatment on tooth No. 14 and referral to an OMFS to assess for the removal of teeth Nos. 15 and 16.
Revealing Possible Concerns
The cases shown in Figure 2 and Figure 3 and Figure 4 through Figure 7 illustrate incidental findings of non-endodontic pathology. Certain incidental findings may simply necessitate informing a patient of a condition without the need for intervention. Others may impact existing treatment plans, such as resorption noted on a tooth being investigated for endodontic pathology and treatment. Still other incidental findings, such as maxillary sinus pathology or jawbone radiolucencies suggesting a cyst or tumor, may warrant specialty referral for further assessment and management. Incidental findings may raise concern of benign or more serious conditions that require urgency in their workup. All incidental findings can introduce complexities to diagnosis and warrant thoughtful discussions with patients.
Conclusion
While not all incidental findings may result in an altered course of treatment, it is critical to evaluate the entirety of a small CBCT scan and manage each case appropriately. Through these scans, patients can be visually informed of these incidental findings and expand their team of healthcare providers if necessary. CBCT scans have greatly advanced the scope of care within the field of endodontics, and it is critical to continue dissecting all of the valuable information that each scan provides.
About the Authors
Jenna Zhu, DMD
Harvard School of Dental Medicine, Boston, Massachusetts
Brooke Blicher, DMD, Certificate in Endodontics
Assistant Clinical Professor, Department of Endodontics, Tufts University School of Dental Medicine, Boston, Massachusetts; Lecturer, Department of Restorative Dentistry and Biomaterials Science, Harvard School of Dental Medicine, Boston, Massachusetts; Private Practice limited to Endodontics, White River Junction, Vermont
Rebekah Lucier Pryles, DMD, Certificate in Endodontics
Assistant Clinical Professor, Department of Endodontics, Tufts University School of Dental Medicine, Boston, Massachusetts; Lecturer, Department of Restorative Dentistry and Biomaterials Science, Harvard School of Dental Medicine, Boston, Massachusetts; Private Practice limited to Endodontics, White River Junction, Vermont
References
1. Ee J, Fayad MI, Johnson BR. Comparison of endodontic diagnosis and treatment planning decisions using cone-beam volumetric tomography versus periapical radiography. J Endod. 2014;40(7):910-916.
2. Special Committee to Revise the Joint AAE/AAOMR Position Statement on use of CBCT in Endodontics. AAE and AAOMR joint position statement: use of cone beam computed tomography in endodontics 2015 update. Oral Surg Oral Med Oral Pathol Oral Radiol. 2015;120(4):508-512.
3. Cağlayan F, Tozoğlu U. Incidental findings in the maxillofacial region detected by cone beam CT. Diagn Interv Radiol. 2012;18(2):159-163.
4. Pette GA, Norkin FJ, Ganeles J, et al. Incidental findings from a retrospective study of 318 cone beam computed tomography consultation reports. Int J Oral Maxillofac Implants. 2012;27(3):595-603.
5. Price JB, Thaw KL, Tyndall DA, et al. Incidental findings from cone beam computed tomography of the maxillofacial region: a descriptive retrospective study. Clin Oral Implants Res. 2012;23(11):1261-1268.
6. Allareddy V, Vincent SD, Hellstein JW, et al. Incidental findings on cone beam computed tomography images. Int J Dent. 2012;2012:871532.
7. de Paula-Silva FW, Wu MK, Leonardo MR, et al. Accuracy of periapical radiography and cone-beam computed tomography scans in diagnosing apical periodontitis using histopathological findings as a gold standard. J Endod. 2009;35(7):1009-1012.
8. Oser DG, Henson BR, Shiang EY, et al. Incidental findings in small field of view cone-beam computed tomography scans. J Endod. 2017;43(6):901-904.
9. Langella J, Finkelman MD, Alon E, et al. Incidental findings in small field of view cone-beam computed tomography scans, Part 2: interpretation with aid of a checklist. J Endod. 2023;49(4):390-394.
10. Rai S, Misra D, Prabhat M, et al. Unintended and unexpected incidental findings on cone beam computed tomography: a retrospective study of 1500 scans. J Indian Acad Oral Med Radiol. 2018;30(3):223-229.