Silver Diamine Fluoride: A Missing Link for Predictable Restorations
Ryan L. Quock, DDS
ABSTRACT
Resin composite offers the ability to restore form and function to teeth in an esthetic, conservative, and durable manner. Success of resin composite depends not only on meticulous bonding and placement technique, but also on minimizing the occurrence of secondary caries. Addressing primary caries first at its root causes and risk factors, prior to restoration, lays the groundwork for the most predictable results. Silver diamine fluoride fits firmly into this paradigm by achieving targeted arrest of active carious lesions and, as a result, is quite compatible with esthetic restorative outcomes, making it an indispensable part of any dental practice.
Direct restoration of form and function to lost tooth structure is a central service of many dental practices, and resin composite has become arguably the most frequently used material for these restorations. Esthetics and wear properties, combined with the ability for conservative preparation design and reparability, make composite attractive to both patients and practitioners. Even though it has been decades since the introduction of adhesive resin chemistry to dentistry, courses in predictable composites remain staples at dental meetings. This is quite understandable, as the technique sensitivity of placing a resin composite cannot be overemphasized.
This article examines a sometimes forgotten barrier to clinical success in composites: the caries process itself. Dentists consistently cite secondary caries as a leading reason for resin composite failure and subsequent replacement.1,2 So, the question is, can anything be done to mitigate this? The key to avoiding secondary caries and thus improving outcomes for resin composite lies in managing and arresting the primary caries first, prior to restoration.3 When primary disease is treated before restoration, the chance of recurrent disease is greatly reduced and the ideal dental environment is created for successful resin composites.
The Foundational Importance of Caries Risk
Resin composite as a restorative material is generally recommended for patients with a low risk for caries.4 Indeed, it has been suggested that a relative contraindication for posterior composite is when a patient has a high caries risk level and is noncompliant with oral hygiene instructions, citing the frequency of secondary caries accompanying restoration failure.5 Alternative materials from the glass-ionomer family are typically suggested for patients with a high caries risk designation.4
If restorative material choice is linked to caries risk level, then it makes sense to briefly consider what caries risk is, how it might be determined, and how it may drive caries management. At a basic level, caries risk is simply a prediction of how likely a patient will manifest dental caries in the near future. Research suggests that certain patient factors (such as fluoride use) protect against caries, while others (such as frequent snacking) increase risk for caries; the presence of current, active dental caries is a strong statistical predictor of future caries activity and almost certainly places the patient in a high caries risk category.6
Thus, the following dilemma is clear: The patient with cavitated active carious lesions may indeed need restorations to eliminate a niche for plaque accumulation and return to form/function. However, at the same time, those very lesions (and the associated risk factors) make the patient high risk for caries, thus contraindicating the use of composite for restoration. Placing composite into a cavity without treating the underlying etiology (dental caries) will not do much for the disease and the tooth will likely be at risk for secondary caries. Indeed, removal of "all the carious dentin" during tooth preparation does not eliminate all of the cariogenic bacteria in the dentin tubules nor the patient risk factors that contributed to the disease. This leaves the conscientious, evidence-based practitioner in a predicament.
Addressing Disease and Its Etiology
Dental caries involves bacterial metabolism of dietary carbohydrates resulting in acid by-products; prolonged low pH due to these acids leads to gradual mineral content loss from tooth structure. As it is currently understood, the caries process is like a pendulum that has swung too far to a low-pH environment, which, unfortunately, tends to be the optimal breeding ground for the acid-producing cariogenic bacteria that create and perpetuate that low-pH environment.7 In patients with normal salivary presence, this vicious cycle, which tends to be similar across the age spectrum, can be broken by interventions that swing the pH balance to a more neutral realm. Such interventions may include dietary counseling and behavior modification, plaque management, and intentional exposure to appropriate fluoride modalities. Approaches like these both manage the disease and help lower the caries risk level.6
In short, the logical and reasonable approach to avoiding secondary caries (and, as a result, setting the patient up for more predictable composite restorations) is to manage the primary caries first. This approach is similar to that taken by many orthodontists, who may refuse to start braces, or will pause mid-treatment, until the patient's disease is under control. Orthodontists do not want caries to confound their patient outcomes, and neither should restorative dentists.
For high caries risk patients (ie, those with active carious lesions) a multi-pronged approach is indicated to manage disease. Risk factors, such as snacking/sugary beverage habits and plaque accumulation, need to be addressed with patient education and empowerment and monitoring for improvement. Protective factors, such as prescription of 5,000 ppm fluoride toothpaste and regular in-office fluoride varnish, need to be part of the treatment plan.6 Also, active carious lesions need to be dealt with in a manner that maximizes caries arrest.
Acute treatment per tooth/surface to optimize caries arrest will vary and critically depends on each lesion's clinical presentation. Non-cavitated lesions (structurally intact but likely discolored) have the inherent potential for arrest with a nonsurgical approach, including the aforementioned topical fluoride approaches and improved patient oral health habits, and restoration is not indicated. Cavitated lesions (a hole or empty space resulting from irreversible tooth substructure loss) whose locations are non-cleansable by saliva/brushing may benefit most from immediate restoration to eliminate the protected bacterial niche. If this is the case, the use of glass-ionomer or resin-modified glass-ionomer (RMGI) to restore may be considered, because these materials release fluoride to combat the caries process, and especially because resin composite is contraindicated for high-risk patients.5
By contrast, for cleansable cavitated lesions, silver diamine fluoride (SDF) is an evidence-based, American Dental Association-recommended modality that has the ability to arrest carious lesions.8 Its usage sets up the clinician to restore with resin composite confidently at a later time when the disease activity and risk level is reduced. SDF likely has a place in every restorative dental practice.
Facilitating Predictable Restorations
Thirty-eight percent (38%) SDF is a basic solution (pH ≥9-10) of silver and fluoride ions stabilized in ammonia. This synergistic combination inhibits biofilm growth and various matrix metalloproteinases and results in a resistant silver chloride precipitate on carious dentin.9 The clinical effect is that SDF arrests8 and prevents caries across the age spectrum, from children to adults.10,11 That is, if SDF is applied to an accessible, cleansable carious surface on any tooth, there is a strong likelihood that the lesion will arrest.
The implication of SDF for effective caries management (and restorative dentistry) is profound. The practitioner and patient can work together to re-balance the caries risk level by increasing protective factors (fluoride exposure) and decreasing risk factors (diet and hygiene), and current disease activity can be acutely halted with SDF. The summary accomplishment of this holistic approach is an oral environment that favors health and, significantly, is a more appropriate palette for restorative success. Secondary caries is less likely because the primary caries and associated risk factors are actually being addressed.
The technique for SDF application for caries management is quick and easy, and detailed instructions for a variety of scenarios are published elsewhere with free access.12 In short, after receiving appropriate informed consent and achieving reasonable isolation, the clinician simply dips a bendable micro-applicator into the SDF solution and scrubs it onto the target carious surface(s) without tooth structure removal, aiming for 1 minute per lesion.
Because the goal of SDF treatment is to arrest the primary caries first as part of an overall disease control plan, restoration with resin composite is not recommended for placement during the same appointment as SDF application. This allows the patient and practitioner to monitor the arrest progress of the lesion over time as it interacts beneficially not only with the components of the SDF but also patient saliva, in-office fluoride varnish treatments, and improved patient hygiene and habits. Witnessing the arrest of an active carious lesion by meaningful interventions is both powerfully educational (and motivational) for the patient and reassuring for the restorative dentist. If it is determined that a restoration is necessary the same day as SDF application, for reasons such as a carious lesion being located in an uncleansable area or an inability for patient recall, then a glass-ionomer or RMGI restoration is indicated because such materials contribute to primary disease arrest and prevention.12
If resin composite restorations are planned, progress of the caries arrest should be monitored and SDF reapplied to the lesion(s) as needed until a satisfactory level of arrest (and patient oral health status) is achieved. The characteristic darkening of the lesion due to silver precipitation is actually a clinical sign that SDF is "doing the work" of arrest. Typically, this visual cue is accompanied by a noticeable hardening of dentin lesion surfaces via tactile examination.
It is important to understand the color changes that accompany SDF treatment. First, SDF only visibly acts on carious lesions (ie, actively demineralizing areas) of enamel and dentin; all surrounding "sound" tooth structure will remain cosmetically unaffected by silver precipitation. Also, most active carious lesions, especially those that are cavitated and into dentin, are already quite discolored by the disease process; thus, SDF simply makes an existing brownish dentin surface darker. Lastly, SDF-treated lesions, of course, can be restored quite esthetically with resin composite (or other material of choice), making any signs of dentin darkening "disappear."
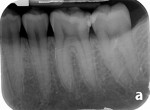
The number and frequency of SDF applications prior to restoration will depend in part on the timeline for desired restoration. If there is urgency to restore (and the patient is motivated and compliant with oral hygiene instructions), arrest can be achieved faster with multiple applications in the first month or so, spaced apart 1 to 2 weeks starting at baseline. For a less urgent or undefined restoration timeline, SDF may be applied at least every 6 to 12 months (Figure 1 and Figure 2).12 In this scenario, it is recommended and convenient for SDF reapplications to coincide with fluoride varnish recall application appointments; first, SDF is applied to the indicated lesions, and then fluoride varnish is immediately applied to all teeth surfaces in the same visit.
Once the restoring dentist has determined that arrest has been achieved and the patient's oral health status is improved, restoration with resin composite can proceed. Because the operator is dealing with arrested lesions, sound conservative principles should be followed. Enamel margins and external walls (including the dentinoenamel junction [DEJ]) should be carefully prepared to remove previously demineralized and/or silver-affected areas. Internal walls (pulpal and axial) can be preserved, including areas that have darkened due to use of SDF (Figure 3 and Figure 4). An RMGI liner (or a glass-ionomer base) can be placed over darkened internal walls as an opaquer, and then etching/bonding/restoring is done (Figure 5 through Figure 8).
Silver Diamine Fluoride's Effect on Bond Strength
Finally, it is appropriate to briefly discuss SDF's effect on bond strength, for which studies show compatibility.13,14 First, however, an earlier premise must be reiterated: When using SDF treatment to arrest the primary caries first as part of an overall disease control plan, same-day restoration with resin composite is not recommended. The disease should be stabilized first, then the clinician can restore later with resin composite when caries risk and activity is reduced. Contextually this is important, because generally speaking the published bonding studies tested for the effect of SDF on immediate bonding to tooth structure. This distinction should be noted when carefully drawing best practices from the available systematic reviews.15,16
Additionally, the variations in sample preparation protocols for the included bonding studies (eg, rinse vs no rinse, phosphoric acid-etch vs self-etch, potassium iodide as a second step or not, etc.) make it necessary to further organize study results by the different approaches used. Once these nuances are accounted for, clearer trends appear that can inform clinical application. In an attempt to be both sufficient and concise in identifying important distinctions, the following is a practical synopsis of the available data:
If restoring the same day as SDF application, rinse and use glass-ionomer. Studies that rinsed the SDF after application but before immediate restoration were less likely to have adverse bonding results.15,16 This was especially true for glass-ionomer when placed over caries-affected dentin treated with SDF, hence the earlier recommendation in this article to use a glass-ionomer-family product directly on SDF-stained, previously carious dentin as an opaquer.
Etch-and-rinse adhesives are preferable to self-etch adhesives. Self-etch adhesives or universal adhesives in self-etch mode consistently reduced the bond strength of resin composite to sound dentin in most studies. By contrast, studies that utilized etch-and-rinse systems after SDF application showed no adverse effect on bond strength to sound dentin, or in one case at least superior bond strengths compared to self-etch groups.15,16
Potassium iodide may interfere with resin composite bond strength. Immediate application of potassium iodide (KI) after SDF has been recommended to reduce discoloration, producing a whitish precipitate. This has yielded equivocal bonding results: In one study the KI step reduced bond strength to dentin while in two studies the KI step had no effect.15,16 This ambiguity, along with the contrasting compatibility of glass-ionomer with SDF-treated dentin, discourages the use of KI as an additional step if restoring with resin composite at this time.
Concluding Remarks
A primary care approach that is framed around first treating dental caries as a disease (etiology and risk) logically leads to more predictable restorative outcomes. This paradigm comes into sharp focus when an esthetic, technique-sensitive material such as resin composite is selected for restoration. Silver diamine fluoride is a potent medical intervention that fits squarely into primary care to arrest and prevent caries, and thus creates the optimal environment for successful resin composite restorations.
DISCLOSURE
The author has previously received educational funding from Colgate and Elevate Oral Care. This article was supported by Centrix Dental.
ABOUT THE AUTHOR
Ryan L. Quock, DDS
Distinguished Teaching Professor, Department of Restorative Dentistry and Prosthodontics, University of Texas School of Dentistry at Houston, Houston, Texas
REFERENCES
1. Da Rosa Rodolpho PA, Rodolfo B, Collares K, et al. Clinical performance of posterior resin composite restorations after up to 33 years. Dent Mater. 2022;38(4):680-688.
2. Mjör IA, Moorhead JE, Dahl JE. Reasons for replacement of restorations in permanent teeth in general dental practice. Int Dent J. 2000;50(6):361-366.
3. Albelasy EH, Hamama HH, Chew HP, et al. Secondary caries and marginal adaptation of ion-releasing versus resin composite restorations: a systematic review and meta-analysis of randomized clinical trials. Sci Rep. 2022;12(1):19244.
4. Direct esthetic restorative materials. In: Powers JM, Wataha JC. Dental Materials: Foundations and Applications. 11th ed. St. Louis, MO: Elsevier Health Sciences; 2017:42-57.
5. Hilton TJ, Broome JC. Direct posterior esthetic restorations. In: Hilton TJ, Ferracane JL, Broome JC, eds. Summitt's Fundamentals of Operative Dentistry: A Contemporary Approach. 4th ed. Hanover Park, IL: Quintessence Publishing; 2013:483-556.
6. Featherstone JDB, Crystal YO, Alston P, et al. Evidence-based caries management for all ages - practical guidelines. Front Oral Health. 2021;2:657518.
7. Zhang JS, Chu CH, Yu OY. Oral microbiome and dental caries development. Dent J (Basel). 2022;10(10):184.
8. Slayton RL, Urquhart O, Araujo MWB, et al. Evidence-based clinical practice guideline on nonrestorative treatments for carious lesions: a report from the American Dental Association. J Am Dent Assoc. 2018t;149(10):837-849.e19.
9. Mei ML, Lo ECM, Chu CH. Arresting dentine caries with silver diamine fluoride: what's behind it? J Dent Res. 2018;97(7):751-758.
10. Chibinski AC, Wambier LM, Feltrin J, et al. Silver diamine fluoride has efficacy in controlling caries progression in primary teeth: a systematic review and meta-analysis. Caries Res. 2017;51(5):527-541.
11. Oliveira BH, Cunha-Cruz J, Rajendra A, Niederman R. Controlling caries in exposed root surfaces with silver diamine fluoride: a systematic review with meta-analysis. J Am Dent Assoc. 2018;149(8):671-679.e1.
12. Young DA, Quock RL, Horst J, et al. Clinical instructions for using silver diamine fluoride (SDF) in dental caries management. Compend Contin Educ Dent. 2021;42(6):e5-e9.
13. Camacho KJ, English JD, Jacob HB, et al. Silver diamine fluoride and bond strength to enamel in vitro: a pilot study. Am J Dent. 2018;31(6):317-319.
14. Quock RL, Barros JA, Yang SW, Patel SA. Effect of silver diamine fluoride on microtensile bond strength to dentin. Oper Dent. 2012;37(6):610-616.
15. Fröhlich TT, Botton G, Rocha RO. Bonding of glass-ionomer cement and adhesives to silver diamine fluoride-treated dentin: an updated systematic review and meta-analysis. J Adhes Dent. 2022;24(1):29-38.
16. Jiang M, Mei ML, Wong MCM, et al. Effect of silver diamine fluoride solution application on the bond strength of dentine to adhesives and to glass ionomer cements: a systematic review. BMC Oral Health. 2020;20(1):40.