The Dental Fluoridation Potential of Drinking Water
Karissa Renyer, BS; and Phil McFadden, PhD
ABSTRACT
Water fluoridation is commonly cited as one of the greatest health achievements of the 20th century because of its effectiveness in reducing the incidence of dental caries. Despite the breadth of research on the subject, little is known about how variation in the composition of municipal water may affect the uptake of fluoride by tooth enamel. This study addressed this issue by developing a model system for testing fluoride uptake into hydroxyapatite, the primary mineral of tooth enamel, to investigate how varying water composition influences fluoride uptake. The tested water variables included the pH and degree of water hardness. A representative experiment involving several municipal water sources then examined how this approach can be used to measure fluoride uptake from any sample of drinking water. Aside from an optimal pH of 6 to 7 for fluoride uptake, there was a remarkable constancy to the uptake of fluoride by hydroxyapatite from the many water samples evaluated. These findings, therefore, suggest that for a given individual's personal history, any observed variation in enamel fluoridation is less likely to be the result of variation in the composition and geographical source of the fluoridated water and more likely a consequence of individual behavioral and biological factors that conceivably affect fluoride uptake into tooth enamel.
Lack of a healthy diet and access to quality dental care creates many issues that negatively impact both oral and overall health and that can escalate to create costly health problems.1 It is imperative for affordable dental products to be available to the public. Though not a traditional dental product, community water fluoridation has been shown for decades to reduce the prevalence of dental caries, the most common chronic disease in children.2,3 Specifically, fluoridated water has been shown to reduce caries incidence by 27% in adults and 34% in children.4,5 The Centers for Disease Control and Prevention (CDC) has found fluoridated water to be the most cost-effective and efficient way of providing the benefits of fluoride to the general population, regardless of age, income, or degree of education.6 The CDC cites 0.7 ppm as the optimal fluoride content of drinking water to balance the benefits of decreased tooth decay with the risks of dental fluorosis.7 Maintaining a healthy oral cavity is a key component of achieving overall health and well-being, and fluoridated drinking water is an essential way of helping protect the oral health of the public.
Fluoride becomes incorporated into the plaque of the mouth, as a reservoir, then becoming part of the oral biofilm.8 As proteins precipitate and attach to the tooth surface, the negatively charged proteins attract calcium ions and form a bridge in the pellicle layer. The calcium ions also attract negatively charged fluoride ions, and the resulting calcium fluoride becomes the bioavailable source of fluoride. When the pH drops below the critical pH of enamel, about 5.5, the enamel undergoes demineralization on the surface as nanoparticles of hydroxyapatite dissociate from the surface layer.
Fluoride provides protection against the loss of enamel in two different ways. First, saliva is supersaturated with nanocrystallites of hydroxyapatite. When the oral pH is greater than 5.5 (the critical point), remineralization occurs as these crystallites fill the micropores in the enamel that are formed during periods of low oral pH,8 by a process of oriented attachment. Fluoride aids in this process by converting nanoparticles of hydroxyapatite into fluorapatite, resulting in enhanced remineralization of the enamel.8 Secondly, at pH values above the critical point, fluoride also tends to become incorporated in enamel by directly replacing the hydroxyl group of hydroxyapatite particles in the surface of the enamel, again forming fluorapatite.8 Fluorapatite has a lower solubility than hydroxyapatite, which increases its range of acid resistance to pH 4.5.9 The fluoridated enamel has increased protection against demineralization. Fluoride also has antimicrobial effects via its ability to interfere with enzymatic functions; this has been proposed to lessen caries incidence by reducing the degree of acid formation by cariogenic bacteria.9
Hydroxyapatite comprises 70% to 80% by weight of tooth enamel and dentin.10 It is a durable mineral arranged as hexagonal fibers that lend compressive strength and hardness.10 Low pH (eg, below 5.5) is well-known to etch hydroxyapatite from tooth enamel as a prelude to tooth decay.3 Supplemental hydroxyapatite has long been used in medicine and dentistry for bone repair and dental therapies.10 Nanoparticle hydroxyapatite (<50 nm) is now produced that is similar in size to hydroxyapatite crystals naturally present in teeth (25 nm thick, 40 nm to 120 nm wide, and 160 nm to 1000 nm long).10 Recent dental research has shown these artificial nanoparticles of hydroxyapatite to be effective in aiding the natural remineralization process of tooth enamel.11 This has led to its incorporation in various dental products, such as toothpastes, to aid in caries prevention.12
In the following investigation, hydroxyapatite was employed to address the question of how the components of drinking water affect fluoride uptake.
Purpose/Objective
Because drinking water constitutes a significant source of oral fluoride for many people, it is necessary to understand how the composition of municipal water affects the process of fluoride uptake into hydroxyapatite. This study investigated how pH and water hardness (calcium carbonate content) affect fluoride uptake. Additionally, because water composition varies based on the source of the water and the processes used at each municipal water treatment facility, water samples from around the state of Oregon and the United States were compared in their effect on fluoridation of hydroxyapatite.
Materials/Methods/Design
Nanoparticle hydroxyapatite (Fluidinova, fluidinova.com) was used as a surrogate for tooth enamel by centrifuging it into a compact pellet form (Figure 1). A suspension of hydroxyapatite (33 mg in 1 mL ultrapure water) was centrifuged in microcentrifuge tubes to form a compact mineral pellet, which was then exposed to various synthetic compositions of fluoridated drinking water. All samples were placed on a rotating tube mixer and rotated end over end, creating an artificial swish. After the swish, the synthetic drinking water was transferred to a larger centrifuge tube and diluted in a 1:3:8 ratio with ultrapure water and conditioning buffer, respectively, and then measured with a fluoride ion selective electrode. The buffer contained trans-1,2-diaminocyclohexane-N,N,N′,N′-tetraacetic acid monohydrate (CDTA), which helped free fluoride ions from cations that may have interfered with the measurement of fluoride ions.13 A fluoride ion selective electrode was used in conjunction with a calibration curve to determine the final concentration of fluoride remaining in the synthetic water after exposure to hydroxyapatite.
Results
Initial findings revealed that fluoride uptake into hydroxyapatite was a very efficient system, with up to 95% uptake in 90 minutes (Figure 2).
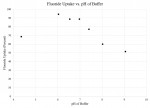
The pH of the solution had a clear effect on the uptake of fluoride by hydroxyapatite. Certain pH values in the pH 6 to 7 range had upwards of 88% of fluoride removed from the synthetic water (Figure 2). There was a reduction in fluoride uptake at pH values lower and higher than that range. The effect appeared to be due to the pH itself rather than the chemical composition or strength of the pH buffer since another study (not shown) that used different buffering concentrations gave a similar pH optimum for fluoride uptake.
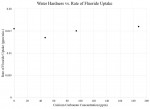
Next, water hardness was investigated under a shorter time interval. There was no significant difference in the rate of fluoride uptake between different degrees of hardness (Figure 3). (Hard water was prepared as per US Environmental Protection Agency [EPA] guidelines.14) This indicates water hardness did not significantly impact fluoride uptake into teeth.
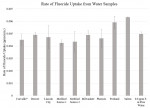
To study how the varying compositions of drinking water in different municipalities may affect the fluoridation of tooth enamel, the hydroxyapatite model system was investigated with nine drinking water samples from varying locations, as follows (list includes sample location, original fluoride concentration [ppm], fluoridation status, and publicly reported water hardness [calcium carbonate concentration] [ppm] of each source of water):
- Corvallis, OR, 0.65, artificially fluoridated, hardness: 23.315
- Denver, CO, 0.45, artificially fluoridated, hardness: 40-12016,17
- Lincoln City, OR, 0.020, naturally fluoridated, hardness: undisclosed
- Medford, OR (Source 1, Big Butte Springs), 0.085, naturally fluoridated, hardness: 4218
- Medford, OR (Source 2, Rogue River), 0.060, naturally fluoridated, hardness: 3018
- Milwaukee, WI, 0.43, artificially fluoridated, hardness: 13719,20
- Phoenix, AZ, 0.80, artificially fluoridated, hardness: 171-27721
- Portland, OR, 0.015, naturally fluoridated, hardness: 3-822
- Salem, OR, 0.53, artificially fluoridated, hardness: 15-1823
Because the fluoride concentrations varied in these samples, the fluoride concentrations were adjusted to the same starting value (0.8 ppm) before proceeding with the experiment. When hydroxyapatite pellets were swished with these samples, the rate of fluoride uptake did not vary significantly, regardless of which municipality the sample originated from (Figure 4), nor did any sample differ appreciably from a control sample of laboratory pure water that had been supplemented with 0.8 ppm fluoride.
Discussion
This study shows that fluoride uptake by hydroxyapatite, the major mineral in tooth enamel, is not affected to any large degree by the typical variations in the chemical composition of drinking water. Aside from the pH optimum of 6 to 7 that was determined, the uptake of fluoride was found to be remarkably resilient to variations in the concentration of the pH buffer, the presence of hardness factors, and the diversity of compositions of municipal waters from different geographical locales.
The optimal pH for fluoride uptake is in the range of pH 6 to 7 (Figure 2). US EPA regulations require the pH of municipal drinking water to be between 6.5 and 8.5.24 As an isolated question, this could indicate that for drinking waters having a pH greater than neutrality, a relatively higher supplementation with fluoride could ensure that the full benefit of fluoride uptake by tooth enamel is achieved; conversely, waters at lower pH than neutrality might withstand having less fluoride supplementation to accomplish desired health benefits. In general, while there is currently no strict consensus view of the amount of fluoride uptake that is optimally beneficial, the results of this study's tests with hydroxyapatite suggest that pH adjustment could provide a method to adjust the uptake of fluoride. Interestingly, water hardness factors did not have any strong effects on the uptake by hydroxyapatite of fluoride at typical supplemental concentrations. Thus, variations in the most common monovalent and divalent cations, as well as the carbonate anion, might not be relevant to the efficiency of the fluoridation of tooth enamel by fluoride-supplemented drinking water. In summary, this knowledge about pH and hardness factors could be of future value as municipalities make or change their decisions regarding how to best supplement their drinking water with fluoride.
While there are certainly variations in drinking waters from source to source, this study rejected geographic dependence of fluoride uptake across numerous distinct locales. The compositions can be presumed to vary, given that, for example, Denver, Milwaukee, Phoenix, and Portland obtain their water from widely separate sources on the continent, and the smaller municipalities from Oregon (Corvallis, Lincoln City, Medford, and Salem) obtain their water from different river basins having distinct geologies. This is notable because it suggests that for far-ranging drinking waters, if supplemented with fluoride, the rate of fluoride uptake by hydroxyapatite, and presumably teeth, will be similar.
Conclusion and Clinical Implications
There is continuing interest in community water fluoridation policy, including questions about the optimum level of fluoride supplementation of drinking water.25 The results of this study are applicable to the conversations that clinicians have with their patients and the community. Dental health professionals can now expand their understanding of the fluoridation process to include the findings of this study; when water chemistry was varied, pH 6 to 7 was optimal for fluoride uptake, and both water hardness and geographic location of a water source had no significant impact. The presence of fluoride in drinking water is a key component of caries risk assessment, and fluoridated water is a valuable tool that communities should utilize. Additionally, the remarkable resilience of fluoridation may indicate that some degree of oral health variation may be the result of individual biological and lifestyle factors as opposed to varied water composition.
DISCLOSURE
Ms. Renyer completed this work toward fulfillment of her Oregon State University Honors College thesis. Dr. McFadden mentored the work.
About the Authors
Karissa Renyer, BS
DMD candidate at Oregon Health and Science University School of Dentistry, Portland, Oregon
Phil McFadden, PhD
Associate Professor, Department of Biochemistry and Biophysics, College of Science, Oregon State University, Corvallis, Oregon
References
1. Fiorillo L. Oral health: the first step to well-being. Medicina (Kaunas). 2019;55(10):676.
2. Benjamin RM. Oral health: the silent epidemic. Public Health Rep. 2010;125(2):158-159.
3. Faller RV, Noble WH. Protection from dental erosion: all fluorides are not equal. Compend Contin Educ Dent. 2018;39(3):e13-e17.
4. Griffin SO, Regnier E, Griffin PM, Huntley V. Effectiveness of fluoride in preventing caries in adults. J Dent Res. 2007;86(5):410-415.
5. Do LG, Spencer AJ. Risk-benefit balance in the use of fluoride among young children. J Dent Res. 2007;86(8):723-728.
6. Centers for Disease Control and Prevention. Community water fluoridation. CDC website. January 15, 2020. https://www.cdc.gov/fluoridation/index.html. Accessed March 11, 2022.
7. Centers for Disease Control and Prevention. Over 75 years of community water fluoridation. CDC website. March 18, 2021. https://www.cdc.gov/fluoridation/basics/anniversary.htm. Accessed March 18, 2022.
8. Ten Cate JM, Buzalaf MAR. Fluoride mode of action: once there was an observant dentist. J Dent Res. 2019;98(7):725-730.
9. Kanduti D, Sterbenk P, Artnik B. Fluoride: a review of use and effects on health. Mater Sociomed. 2016;28(2):133-137.
10. Habibah TU, Amlani DV, Brizuela M. Hydroxyapatite dental material. In: StatPearls[Internet]. Treasure Island, FL: StatPearls Publishing; 2020.
11. Kutsch VK, Chaiyabutr Y, Milicich G. Reconsidering remineralization strategies to include nanoparticle hydroxyapatite. Compend Contin Educ Dent. 2013;34(3):170-176.
12. Fluidinova. Hydroxyapatite properties, uses, and applications. Fluidinova website. https://www.fluidinova.com/hydroxyapatite-properties-uses-and-applications. Accessed March 11, 2022.
13. Metrohm. Determination of fluoride with an ion-selective electrode. Application Bulletin 82/5 e. Metrohm website. https://www.metrohm.com/en-us/applications/AB-082. Accessed March 11, 2022.
14. US Environmental Protection Agency. Standard Operating Procedure for Preparation of AOAC and OECD hard water and other diluents for preparation of antimicrobial products. February 3, 2017. https://www.epa.gov/sites/production/files/2018-01/documents/mb-30-01.pdf. Accessed March 11, 2022.
15. 2022 Water Quality Report. City of Corvallis. 2022. https://archives.corvallisoregon.gov/public/ElectronicFile.aspx?dbid=0&docid=2604081. Accessed March 18, 2022.
16. 2021 Water Quality Report. Denver Water. 2021. . Accessed March 18, 2022.
17. Thompson T. The ‘hard' truth about soft water. Denver Water. July 27, 2017. https://www.denverwater.org/tap/the-hard-truth-about-soft-water. Accessed March 18, 2022.
18. Medford Water's 2021 Water Quality Analyses. Medford Water. March 2022. https://www.medfordwater.org/SIB/files/Water%20Quality%20Analyses%202021.pdf. Accessed March 18, 2022.
19. 2020 Consumer Confidence Report. Milwaukee Water Works. 2021. https://city.milwaukee.gov/ImageLibrary/Groups/WaterWorks/Consumer-Confidence-Reports/2020MWWConsumerConfidenceReport.pdf. Accessed March 18, 2022.
20. FAQs - Water Quality and Public Health, Water Hardness. City of Milwaukee. https://city.milwaukee.gov/water/customer/FAQs/qualityandhealth/Water-hardness.htm#:~:text=Milwaukee%27s%20water%20is%20considered%20moderately,of%20112%2D142%20mg%2FL. Accessed March 18, 2022.
21. 2020 Water Quality Report. City of Phoenix. https://www.phoenix.gov/waterservicessite/Documents/wsdprimarywqr.pdf. Accessed March 18, 2022.
22. 2020 Drinking Water Quality Report. Portland Water Bureau. https://www.portland.gov/sites/default/files/2020-07/2020-portland-drinking-water-quality-report_web.pdf. Accessed March 18, 2022.
23. 2021 Annual Water Quality Report. City of Salem Public Works Department. 2021. https://www.cityofsalem.net/CityDocuments/water-quality-report-english.pdf. Accessed March 18, 2022.
24. US Environmental Protection Agency. Drinking water regulations and contaminants. EPA website. https://www.epa.gov/sdwa/drinking-water-regulations-and-contaminants. Accessed March 11, 2022.
25. US Dept of Health and Human Services Federal Panel on Community Water Fluoridation. U.S. Public Health Service recommendation for fluoride concentration in drinking water for the prevention of dental caries. Public Health Rep. 2015;130(4):318-331.